Prog Retin Eye Res:中国学者第一期刊发文探讨老年致盲眼病早期干预
2019-01-29 肖洁 科学网
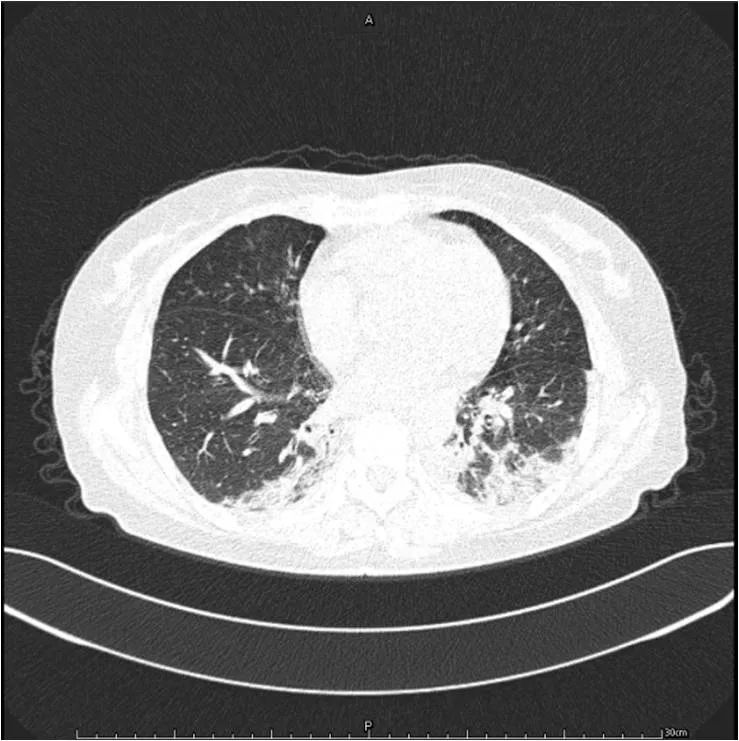
日前,全球眼科领域顶级期刊《Progress in Retinal and Eye Research》(以下简称PRER)在线发表了中南大学爱尔眼科学院教授徐和平及其研究团队的论文《老化视网膜中的免疫调控》。该论文通过探讨老化过程中视网膜的免疫调控,寻求老年性退行性视网膜疾病的发病机理,尝试找到老年黄斑变性、糖尿病视网膜病变等眼病发病早期的干预手段,使致盲眼病患者在不可逆视觉损伤发生之前得到及时的
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#早期干预#
45
#eye#
53
#RET#
33
#眼病#
42
#PRO#
31