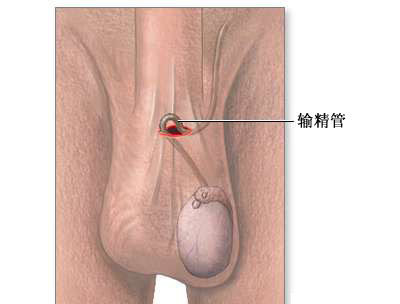
JCO;颠覆!新的研究表明输精管切除术与前列腺癌风险增加无关
2016-09-20 MedSci MedSci原创
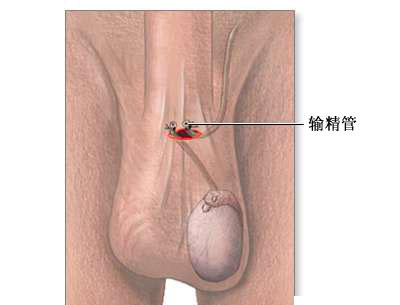
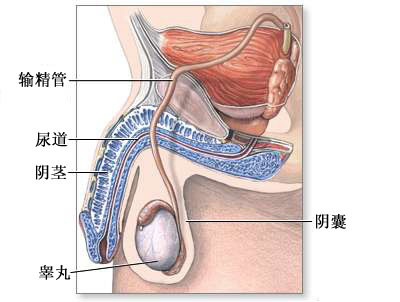
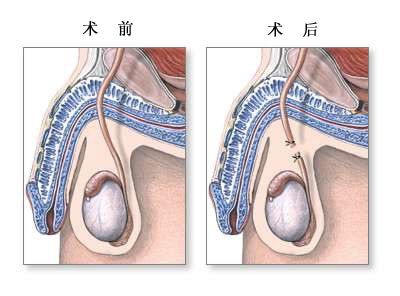
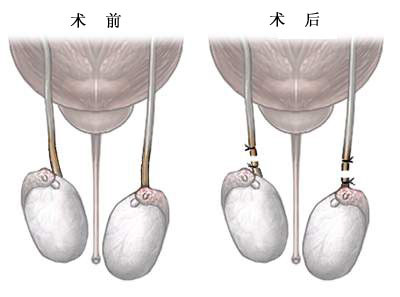
两项美国大型队列研究显示,男性行输精管切除术并没有增加其前列腺癌发生及因前列腺癌死亡的风险。 既往一项前瞻性研究认为行输精管切除术后患前列腺癌的风险增加10%,发生高级别及致命前列腺癌的风险极高,但是其他研究则认为二者并没有联系。 该项新的研究发表于Journal of Clinical Oncology,纳入了参与癌症预防研究Ⅱ的年龄超过40岁的363726位男性,观察输精管切除术和
两项美国大型队列研究显示,男性行输精管切除术并没有增加其前列腺癌发生及因前列腺癌死亡的风险。
既往一项前瞻性研究认为行输精管切除术后患前列腺癌的风险增加10%,发生高级别及致命前列腺癌的风险极高,但是其他研究则认为二者并没有联系。
该项新的研究发表于Journal of Clinical Oncology,纳入了参与癌症预防研究Ⅱ的年龄超过40岁的363726位男性,观察输精管切除术和前列腺癌致死之间的联系。1982-2012年间的随访中共有7451人死于前列腺癌。
结果显示,输精管切除术与前列腺癌死亡率无关:42015名行输精管切除术的男性中,641人死于前列腺癌,相比之下,321711名未行输精管切除术的男性中, 6810人死于前列腺癌[危险比为1.01,(95%可信区间为0.93-1.10)]。
第二个队列研究纳入了参加大型癌症预防试验的营养亚研究的66542名男性,观察,探究输精管切除术是否与前列腺癌的发生率或死亡率有关。其中10589名男性做过输精管切除术,1992-2011年间9133名男性诊断为前列腺癌。
研究人员发现,输精管切除术和总的前列腺癌发病率 (1.02 (0.96 to 1.08)) 或高危级别前列腺癌的发生率 (0.91 (0.78 - 1.07)格里森评分 >8)无关。
该研究的第一作者Eric Jacobs,来自格鲁吉亚亚特兰大美国癌症协会流行病学研究项目,认为“尽管既往研究认为二者之间有关,但我们的结果显示输尿管切除术与前列腺癌发生风险或前列腺癌死亡无关,这或许能够给予考虑行输精管切除术的男性一些安慰”。他还补充道,这是迄今为止验证这个问题的最大研究。
最后他建议,“担心致命性前列腺癌发生的男性应着重关注保持健康的体重,吸烟者应戒烟.肥胖和吸烟都是致命性前列腺癌发生的高危因素,且与其他多种疾病的发生相关”.
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#输精管切除术#
33
#切除术#
36
#输精管#
39
#癌风险#
30
#JCO#
35
#前列腺癌风险#
33
总结的很棒,
41
谢谢分享,继续学习。
52
无论是国际还是国内都是目前肿瘤免疫治疗的研究热点!!总结的很好!!
45