European Radiology:MR黑血血栓成像技术对脑静脉血栓的诊断价值
2022-02-15 shaosai MedSci原创
脑静脉血栓(CVT)是一种相对罕见的脑血管疾病,约占所有脑卒中的0.5-1%。如果能得到及时的诊断和治疗,CV一般预后较好。
脑静脉血栓(CVT)是一种相对罕见的脑血管疾病,约占所有脑卒中的0.5-1%。如果能得到及时的诊断和治疗,CV一般预后较好。CVT的诊断评估主要集中在临床特征和影像检查,如CT静脉成像(CTV)和MR静脉成像(MRV)。然而,由于非特异性的临床表现和静脉解剖变异,往往难以做出快速准确的诊断。
现阶段,黑血MR技术已被广泛用于心脏、深静脉和颅内动脉的成像。最近,有人提出MR黑血血栓成像(BTI)技术对脑静脉系统的血流信号有极好的抑制作用,可直接检测CVT。然而,这种技术主要用于学术研究,且均是在小规模的患者群中进行,因此BTI的现实临床价值仍然未知。
近日,发表在European Radiology杂志的一项研究根据5年的实际临床经验,评估了BTI对疑似CVT患者的诊断价值,为该类患者的早期的诊断及治疗提供了支持。
本研究在2014年至2019年期间对疑似CVT的患者进行了评估。有或没有BTI扫描的患者分别被分为A组和B组。比较了CVT的正确诊断率和可评估的血块年龄的患者。进一步分析了BTI的诊断性能,包括敏感性、特异性和具体分期信息。
在目前的研究中,308名疑似CVT的患者中有221人符合条件(A组114人,B组97人),其中125人被多学科团队诊断为CVT(A组56人,B组69人)。加入BTI图像后,A组的CVT正确诊断率高于B组(94.7% vs 60.8%,P < 0.001,x2 = 36.517)。两组之间具有可评估分期的患者百分比分别为96.4%和33.9%(x2 = 48.191,p < 0.001)。BTI在检测每个病人和每个节段的CVT方面的灵敏度分别为96.4%和87.9%。98.1%的血栓区段可以通过BTI进行分期,其中59.6%与临床分期相符。
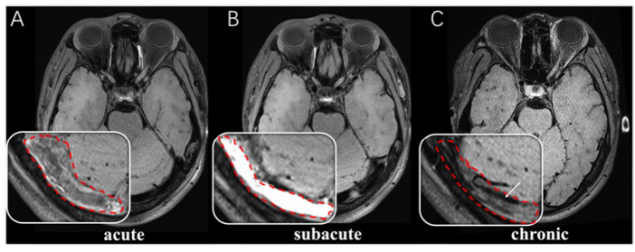
图 处于不同阶段的血栓在BTI上的示例图。轴位BTI图像显示,等信号表明右横窦有急性血栓(A中红色虚线),高信号表明右横窦有亚急性血栓(B中红色虚线),等信号与血流空隙(白色箭头)表明右横窦有慢性血栓(C中红色虚线)。
本研究结果通过对5年的实际临床经验的总结,为BTI在临床实践中的应用提供了强有力的数据支持。在实际的临床实践中,BTI提高了诊断的准确性,并提供了血栓分期的额外信息,这表明该技术可作为快速准确诊断CVT的一个有前途的影像学工具。
原文出处:
Xiaoxu Yang,Fang Wu,Yuehong Liu,et al.Diagnostic performance of MR black-blood thrombus imaging for cerebral venous thrombosis in real-world clinical practice.DOI:10.1007/s00330-021-08286-x
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
41
#静脉血#
50
#诊断价值#
52
#血栓##脑静脉血栓#
71
#静脉#
35
#成像技术#
46