全球首台“胶囊内镜机器人”投入临床使用
2013-03-22 肖鑫 俞治 黄辛 中国科学报
记者在第二军医大学长海医院获悉,由该院联合上海理工大学、武汉安翰光电技术有限公司研制的“胶囊内镜机器人”,已获国家药监局注册审批,并正式投入临床使用。 据查证,这是全球首台可定位可遥控胶囊内镜机器人。患者只要吞下一颗普通胶囊药物大小的胶囊内镜,医生就能把隐藏在患者胃里的病灶看得清清楚楚。 该机器人的总设计师、第二军医大学长海医院消化内科主任李兆申教授介绍说,人体腹中5至7米长的
记者在第二军医大学长海医院获悉,由该院联合上海理工大学、武汉安翰光电技术有限公司研制的“胶囊内镜机器人”,已获国家药监局注册审批,并正式投入临床使用。
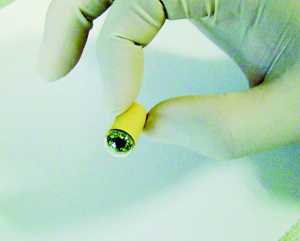
据查证,这是全球首台可定位可遥控胶囊内镜机器人。患者只要吞下一颗普通胶囊药物大小的胶囊内镜,医生就能把隐藏在患者胃里的病灶看得清清楚楚。
该机器人的总设计师、第二军医大学长海医院消化内科主任李兆申教授介绍说,人体腹中5至7米长的小肠,一向是胃镜、肠镜检查所无法涉足的“盲区”。长期以来,我国小肠疾病的诊断率只有10%。
使用“胶囊机器人”检查胃病,患者仅需吞服一粒特制的小“胶囊”,胶囊便会听从医生的无线磁场遥控指令,进入患者肠胃,并按照医生的操控,在患者肠胃中上下左右翻滚、旋转或者平移。同时,一幅幅图片将实时传出体外,收录进一旁的电脑中,供医生分析和诊断。
更具创新性的是,由于安装了磁定位芯片系统,胶囊内镜可以在医生的控制下巡视消化道任意位置,实现定位功能。为此,研究人员开发出一种类此CT扫描仪的“检测床”,让病人吞服胶囊内镜后躺上去,通过体外磁场控制,引导胶囊内镜游走至体内病灶处悬浮。然后,检测人员控制磁场的大小和方向,可以让胶囊内镜拥有仰视、俯瞰、旋转等6个角度的“视角”,充分聚焦消化系统内有何异样。
检查完成后,胶囊将会顺着胃肠道自然排出患者体外,整个胃镜检查过程只需要半个小时。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#临床使用#
43
#内镜#
50
#机器人#
39
#胶囊内镜#
31
#机器#
0