BMC Cancer:探索晚期EGFR/ALK突变非小细胞肺癌(NSCLC)生存超5年患者的临床特征
2022-03-31 yd2015 MedSci原创
在EGFR突变和ALK重排的晚期NSCLC患者长期生存曲线中发现了一个尾部平台,大多数患者都在接受治疗,尤其是EGFR突变的NSCLC。
近期,在BMC Cancer杂志上发表了一项研究成果,主要评估晚期EGFR/ALK突变非小细胞肺癌(NSCLC)患者初始使用化疗时长期生存的临床特征和影响因素。
在2008年12月至2015年9月间接受首次化疗的177例晚期、EGFR突变或ALK重排NSCLC患者被纳入研究。
177例患者中,EGFR突变患者155例,ALK重排患者22例。在整个队列中,中位随访时间为36.9个月(范围0.5-131.4)。EGFR突变患者的中位随访时间为35.5个月(范围0.5-131.4),ALK重排患者的中位随访时间为51.8个月(范围0.8-131.4)。
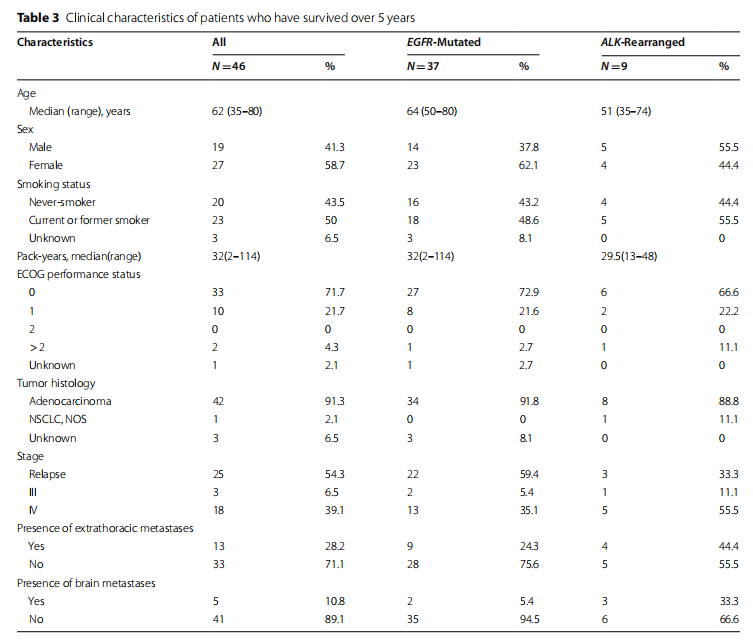
在数据锁定时,EGFR突变NSCLC患者中,17例(10.9%)存活,17例(10.9%)失访,121例(78.0%)死亡。ALK重排患者存活6例(27.2%),失访3例(13.6%),死亡13例(59.0%)。37例(23.8%)EGFR突变患者和9例(40.9%)ALK重排患者存活超过5年。
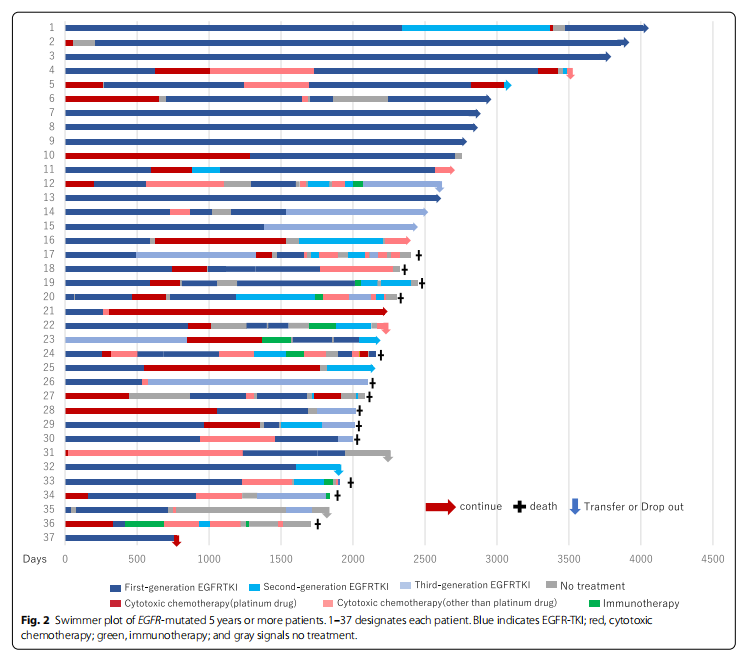
- 在EGFR突变的患者中,EGFR-TKI治疗的中位总持续时间为18.09个月(范围为0-128.61个月);细胞毒性化疗为8.08个月(范围0-64.37个月);免疫治疗为1.34个月(范围为0-9.53个月)。
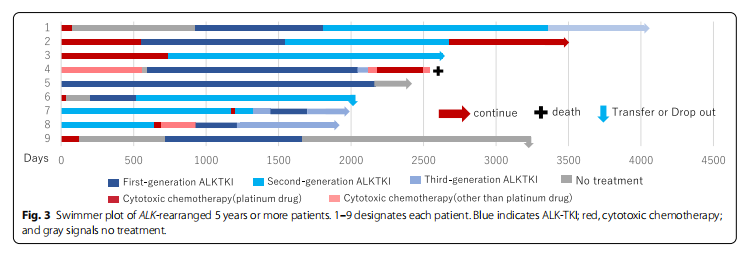
- 在ALK重排患者中,ALK-TKI治疗的中位总持续时间为31.36个月(范围为0-101.87个月);细胞毒性化疗为8.17个月(0-44.18个月);免疫治疗为0.69个月(范围为0-0.69个月)。
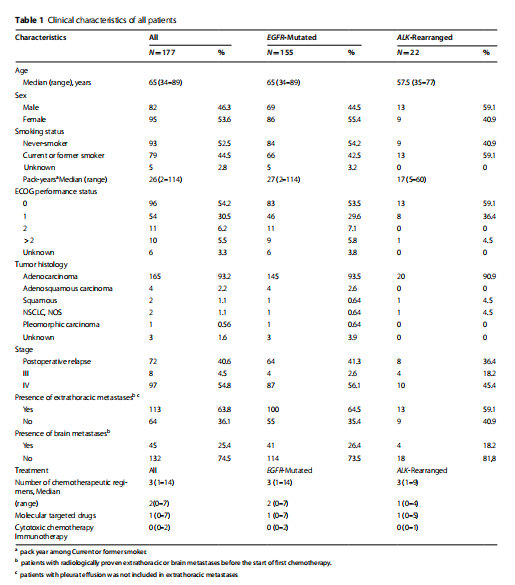
开始一线化疗的中位年龄为65岁(34岁-89岁)。女性(53.6% vs 46.3%)和不吸烟(52.5% vs 44.5%)的比例更高。100例(84.7%)患者ECOG PS为0-121例患者(11.7%)为2或以上。在病理诊断方面,93.2%的患者患有腺癌。177例患者中70例术后复发。发生胸外转移患者113例(63.8%),脑转移患者45例(25.4%)。
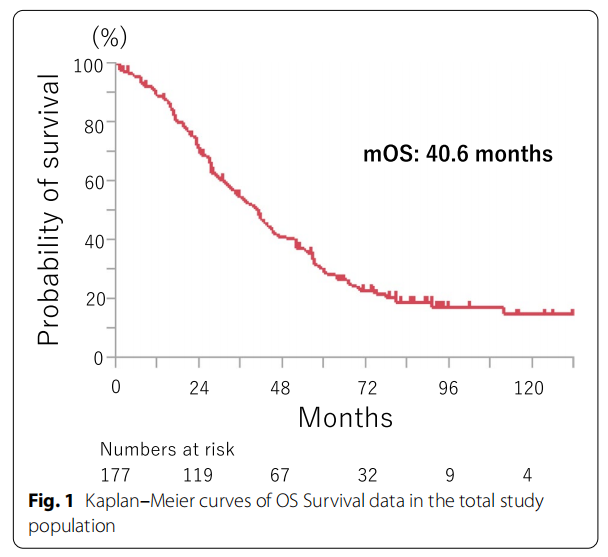
整体人群患者的中位OS为40.6个月,1年生存率为89%,3年生存率为54%,5年生存率为28%。72个月后,OS曲线趋于平稳,此时EGFR突变患者的生存率为20.3 % (95% CI, 13.6 - 27.0)%,ALK重排患者的生存率为46.0 % (95% CI, 24.1 - 67.8) %。EGFR突变患者的中位OS为36.9个月(95%CI, 29.6 - 43.5), ALK重排患者的中位OS为55.4个月(95%CI, 32.9 - 111.3)。
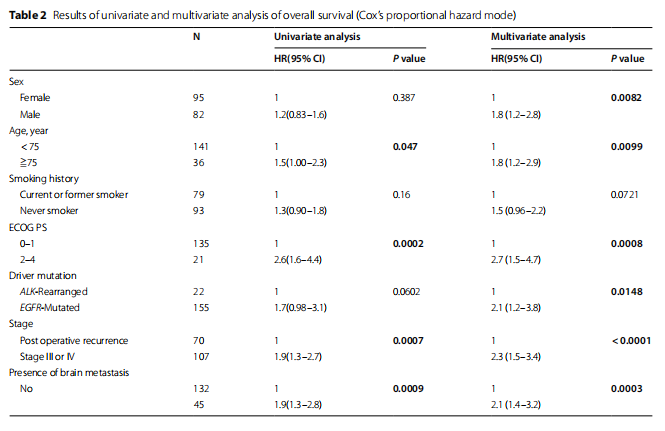
经log-rank检验,5个亚组OS差异均有统计学意义。与OS显著延长相关的变量有:年龄小于75岁(p=0.027), ECOG PS为0或1 (p=0.0002),术后复发(p=0.0015),无胸外转移(p<0.0001),基线时无脑转移(p=0.0009)。
EGFR突变患者各亚型为外显子19缺失74例(47.7%),外显子21 L858R突变63例患者(40.6%),外显子18 G719A / C / S有4例患者(2.6%),外显子L861Q有3例患者。19 del, L858R突变和其他亚组患者的生存无显著统计学差异。
采用Cox比例风险模型进行多因素分析,6个变量与显著延长的OS相关:女性、年龄在75岁以下、ECOG PS为0或1、ALK重排、术后复发和无脑转移。
37例(23.8%)EGFR突变患者和9例(40.9%)ALK重排患者存活超过5年。37例EGFR突变患者中,5名患者中,仅使用一种EGFR-TKI治疗可病情稳定,而在2名患者中,使用两种EGFR-TKI治疗获得病情稳定。在其他患者中,不仅使用EGFR-TKIs,还使用细胞毒性化疗或免疫疗法来控制他们的疾病。在长期生存的病例中,EGFR-TKI的使用时间往往比其他药物更长,一些病例使用更长的EGFR-TKI后存活10年或更长时间。
9例(40.9%)ALK重排患者中,病例1、2、4、9患者在ALK-TKI启动前进行治疗,首次化疗采用细胞毒性化疗。病例7和8是用阿来替尼治疗。在病例3患者采用第二代ALK-TKI获得稳定。在病例5、9患者,停药后病情仍稳定。
综上,研究表明,在EGFR突变和ALK重排的晚期NSCLC患者长期生存曲线中发现了一个尾部平台,大多数患者都在接受治疗,尤其是EGFR突变的NSCLC。
原始出处:
Shimamura SS, Shukuya T, Asao T, Hayakawa D, Kurokawa K, Xu S, Miura K, Mitsuishi Y, Tajima K, Shibayama R, Shimada N, Takahashi F, Takahashi K. Survival past five years with advanced, EGFR-mutated or ALK-rearranged non-small cell lung cancer-is there a "tail plateau" in the survival curve of these patients? BMC Cancer. 2022 Mar 25;22(1):323. doi: 10.1186/s12885-022-09421-7. PMID: 35337281; PMCID: PMC8953392.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#非小细胞#
50
#临床特征#
46
#BMC#
38
#ALK突变#
45
#GFR#
34
积分
33