Anticancer Res:卵巢癌的替代疗法---低剂量加压腹腔内气溶胶化疗 (PIPAC)
2015-04-30 范伟译 MedSci原创
背景:八旬卵巢癌病人局限于腹部可能不愿意或者不能接受全身化疗。低剂量加压腹腔内气溶胶化疗 (PIPAC)与顺铂和阿霉素一起进行腹腔内化疗,可以反复应用,并可能防止系统性化疗产生的副作用。 病例报告:我们分析一个84岁的妇女腹腔镜和组织学证实卵巢癌情况下拒绝接受全身化疗的病例。她接受八个疗程的28 - 104天的低剂量PIPAC与顺铂7.5毫克/米(2)和阿霉素1.5毫克/米(2) 在大气压12毫
背景:八旬卵巢癌病人局限于腹部可能不愿意或者不能接受全身化疗。低剂量加压腹腔内气溶胶化疗 (PIPAC)与顺铂和阿霉素一起进行腹腔内化疗,可以反复应用,并可能防止系统性化疗产生的副作用。
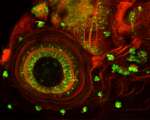
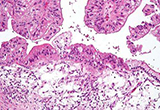
病例报告:我们分析一个84岁的妇女腹腔镜和组织学证实卵巢癌情况下拒绝接受全身化疗的病例。她接受八个疗程的28 - 104天的低剂量PIPAC与顺铂7.5毫克/米(2)和阿霉素1.5毫克/米(2) 在大气压12毫米汞柱下,37°C温度下化疗30min。客观肿瘤反应定义为肿瘤组织学上的复原,疾病稳定通过重复的腹腔镜扫描和腹部计算机断层扫描给出腹膜癌变指数。治疗耐受好,没有常见术语的不良反应(CTCAE)CTCAE > 2。15个月后的随访,病人还活着,临床稳定。生活质量由欧洲癌症研究和治疗组织(EORTC)QLQ-C30进行测量,表明在5 - 6个月(全球物理成绩,全球健康得分,全球生活质量) 得到改善,没有累积增加的胃肠道毒性。
结论: 在老年患者中,低剂量加压腹腔内气溶胶化疗是一种新形式的腹腔化疗,可以多次应用。低剂量加压腹腔内气溶胶化疗可能是另一个替代疗法,耐受性较好,限于腹部那些不能接受全身化疗的老年卵巢癌患者。
原始出处
Giger-Pabst U1, Solass W2, Buerkle B3, Reymond MA1, Tempfer CB. Low-dose Pressurized Intraperitoneal Aerosol Chemotherapy (PIPAC) as an Alternative Therapy for Ovarian Cancer in an Octogenarian Patient. Anticancer Res. 2015 Apr
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#替代疗法#
36
#腹腔内#
33
#低剂量#
26
#气溶胶#
28
值得关注
104