JAMA NEUROLOGY:ARB类药物不仅降低高血压病,而且显著减少癫痫发病率
2022-10-22 MedSci原创 MedSci原创
在这项高血压患者的队列研究中,ARB治疗与癫痫的发生率显著降低有关。
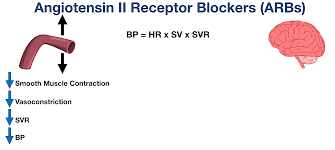
动脉高血压与癫痫的发病率增加有关。动物研究的结果表明,血管紧张素受体阻断剂(ARB)治疗可以抑制癫痫发作。然而,目前缺乏临床数据支持ARB疗法在人类中的应用。该研究的目的是评估ARB治疗是否与高血压患者的癫痫发病率下降有关。
这项队列研究从疾病分析器数据库(IQVIA)中获取了18岁或以上的高血压患者和至少1个降压药物处方的数据。2010年1月至2020年12月期间,患者在德国的1274家普通诊所接受治疗。有1553875名至少开过1种降压药的患者的数据。使用4类抗高血压药物(β-受体阻滞剂BBB、ARBs、血管紧张素转换酶抑制剂ACEI和钙通道阻滞剂[CCBs])中的1类药物治疗的患者使用倾向性评分进行相互匹配。主要结果是与其他抗高血压药物类别相比,与ARB治疗相关的癫痫发病率。
结果该研究总共有168612名患者被纳入倾向性评分匹配中,每个降压药物类别有42153名。患者的平均[SD]年龄为62.3[13.5]岁,21 667人(51.4%)为女性。5年内的癫痫发生率在接受ARB治疗的患者中最低(1年为0.27%,3年为0.63%,5年为0.99%),在接受BBB和CCB的患者中最高(1年时β-受体阻滞剂和CCB均为0.38%;3年时β-受体阻滞剂为0.91%,CCB为0.93%;β-受体阻滞剂为1.47%;5年时CCB为1.48%)。与其他药物类别相比,ARBs治疗与癫痫发病率显著下降23%有关(HR=0.77;95%CI,0.65-0.90)。
在这项高血压患者的队列研究中,ARB治疗与癫痫的发生率显著降低有关。研究结果表明,降压药可作为预防动脉性高血压患者癫痫的一种新方法。
参考文献:
Association Between Angiotensin Receptor Blocker Therapy and Incidence of Epilepsy in Patients With Hypertension. JAMA Neurol. Published online October 17, 2022. doi:10.1001/jamaneurol.2022.3413
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








不知机制何在
32
学习受益,开拓视野
30
#期刊论坛##Nat#
38
不错的文章
39