Infection: 低于12.5 mg/kg/天的低剂量乙胺丁醇治疗不会恶化肺分枝杆菌和胞内分枝杆菌疾病的临床结果
2022-02-17 MedSci原创 MedSci原创
非结核分枝杆菌(NTM)是指结核杆菌及麻风分枝杆菌以外的所有分枝杆菌,也称为环境分枝杆菌。
世界范围内非结核分枝杆菌 (NTM) 的发病率和流行率正在增加,而肺分枝杆菌( M. avium ) 和胞内分枝杆菌( M. intracellulare ) 占 NTM 感染的大部分。患有肺分枝杆菌和细胞内分枝杆菌疾病通常分为两种主要表型:纤维腔 (FC) 和结节性支气管扩张 (NB)。目前的指南推荐多药化疗,包括大环内酯类、乙胺丁醇和利福平,以治疗肺分枝杆菌和细胞内分枝杆菌疾病。乙胺丁醇有时会引起周围神经病变、超敏反应和视神经病变等不良反应,导致治疗中断。一些回顾性研究表明,乙胺丁醇的视神经病变发生率是剂量依赖性的,即 35 mg/kg/天或更多时为 18%,25 mg/kg/天时为 6%,15 mg/kg 时为 1% /天。然而,较低剂量的乙胺丁醇是否会降低微生物治愈和复发结果仍然未知。本研究的目的是评估低剂量乙胺丁醇与临床结果之间的关联,包括阴性培养转化、微生物治愈、不良事件、对大环内酯类药物的耐药性和复发。

为此,研究人员回顾性收集了2016年至2020年间治疗超过 12 个月的非结核分枝杆菌 (NTM) 患者。根据每日乙胺丁醇剂量比较临床结果,包括阴性培养转化、微生物治愈、不良事件、对大环内酯类药物的耐药性和复发。
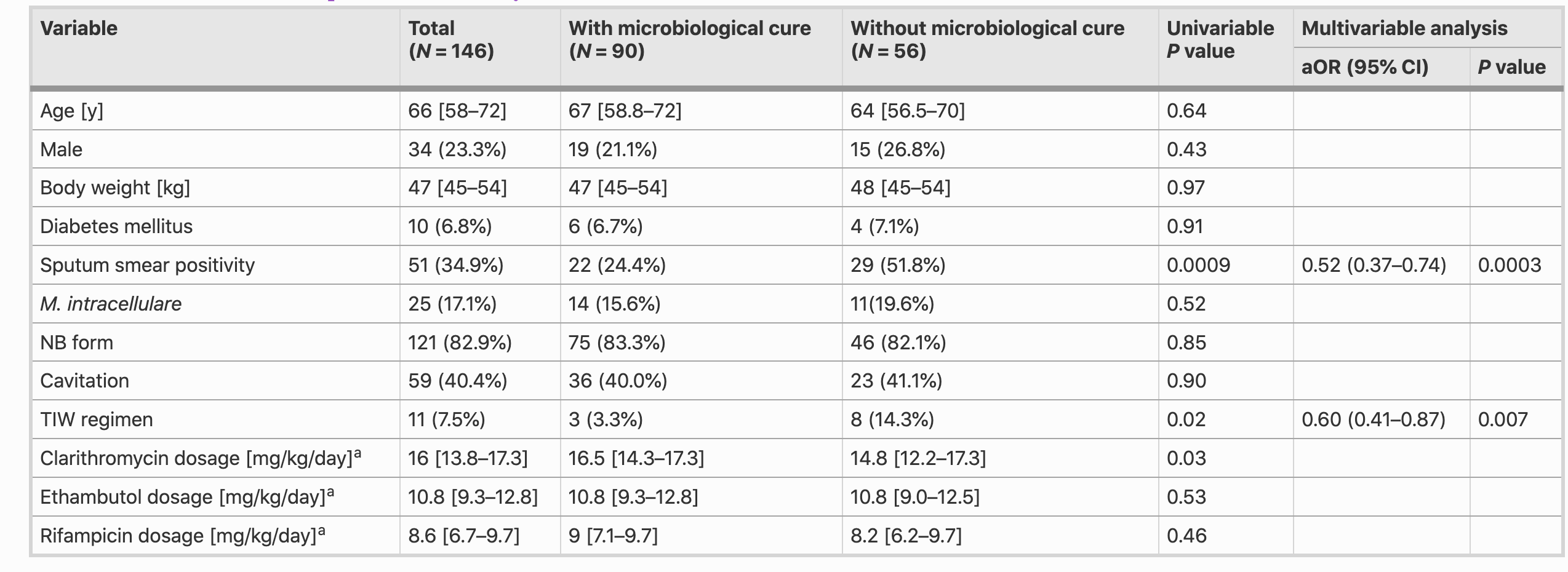
研究结果显示在 146 名患者中,42 名患者接受了超过 12.5 mg/kg/天的乙胺丁醇剂量治疗,104 名患者接受了较低剂量的治疗。培养转阴125例,微生物治愈90例。在获得微生物治愈的 16 名患者中发现了疾病复发。未观察到大环内酯类耐药,培养阴性转化率(P =1.00)或微生物治愈率(P = 0.67)在高剂量和低剂量乙胺丁醇组之间存在差异。痰涂片阳性与阴性培养转换的较低调整优势比 (aOR) 相关 (aOR: 0.48, 95% CI: 0.29–0.80)。微生物治愈的较低 aOR 与痰涂片阳性 (aOR: 0.52, 95% CI: 0.37–0.74) 和使用间歇方案 (aOR: 0.60, 95% CI: 0.41–0.87) 独立相关。每日乙胺丁醇剂量未被确定为任何结果的预后因素。高剂量乙胺丁醇组和低剂量乙胺丁醇组分别有 7.1% 和 1.0% 出现视神经病变(P = 0.07),但没有统计学意义。
本项研究结果证实在基于指南的化疗中,12.5 mg/kg/天或更少的乙胺丁醇剂量可以减少视神经病变而不会恶化临床结果。
原始出处:
Fumiya Watanabe. Et al. Low-dosage ethambutol, less than 12.5 mg/kg/day, does not worsen the clinical outcomes of pulmonary Mycobacterium avium and Mycobacterium intracellulare disease: a retrospective cohort study.Infection.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#临床结果#
47
#分枝杆菌#
42
#低剂量#
0
#Infection#
39