Spine:改良肋横突入路多节段椎体切除术与单节段疗效类似
2013-06-18 Spine 丁香园
多种疾病可以影响脊柱前柱,如肿瘤,病理或非病理性骨折,感染等。通常这类患者需要行椎体切除以获得疾病的患者或治愈。对胸椎而言,行前路椎体切除存在较大风险,因前路手术经过肺,胸部大血管等众多重要结构,任何一个损伤均可能导致患者术后出现严重并发症。因此大部分学者倾向于从后路进行胸椎椎体切除。目前主要有3种常用入路:经椎弓根(transpedicular),肋横突入路(costotransversecto
多种疾病可以影响脊柱前柱,如肿瘤,病理或非病理性骨折,感染等。通常这类患者需要行椎体切除以获得疾病的患者或治愈。对胸椎而言,行前路椎体切除存在较大风险,因前路手术经过肺,胸部大血管等众多重要结构,任何一个损伤均可能导致患者术后出现严重并发症。因此大部分学者倾向于从后路进行胸椎椎体切除。目前主要有3种常用入路:经椎弓根(transpedicular),肋横突入路(costotransversectomy),外侧腔外入路(lateral extracavity)。在传统观念中,部分需要行多节段椎体切除的患者手术风险,术后并发症发生的可能性均较单节段高,因此对需要多节段切除胸椎椎体的患者术者往往选择采用前入路。但事实上目前并没有后路单节段或多节段椎体切除两者手术效果的直接比较研究,近日由美国密歇根大学研究者完成的一项对改良后路肋横突入路行单节段或多节段胸椎椎体切除患者回顾性对比研究发现,单或多节段胸椎椎体切除的患者手术效果无显著差别,相关结论发表于spine杂志上。
研究者回顾性分析了2006年-2009年接受改良后路肋横突入路单节段或多节段椎体切除术治疗脊柱疾病的患者电子数据,收集指标包括:患者人口统计学基线数据,如年龄,BMI,性别,内科疾病史,术前疾病诊断(肿瘤,感染,创伤);为评估患者术前功能情况,记录术前肌力及神经功能状态(MRC评分,medical research council,Nurick评分),疼痛等指标;患者术中各项指标,如手术时间,术中失血,是否需要输血,输血量,术中、术后30天内并发症等指标。
术后4、6周,3月,1年,后每年门诊随访神经功能恢复和影像学X片。同时记录患者术后再手术率,功能恢复,肌力,神经功能状态,疼痛等情况。
手术方法:
患者俯卧位,建立术中神经监测。在手术节段正中线行正中皮肤切口,骨膜下剥离,暴露后侧脊柱结构。在目标椎体的近、远端至少2个椎体中置入椎弓根螺钉,通过Snell和Yoo等人创立的改良后路经肋骨横突切除入路,以Overby和Rothman等人介绍的方法行椎体切除。如有必要,则对侧开口,辅助完全切除椎体(图1)。完全切除椎间盘,刮除椎体终板为后期植骨准备。若行多椎体节段切除,则采用相同入路重复上述过程(图2)。在椎体切除节段放置钛融合器。除T12及L1节段外,在放置融合器时可分离向外行走的神经以方便融合器的放置。
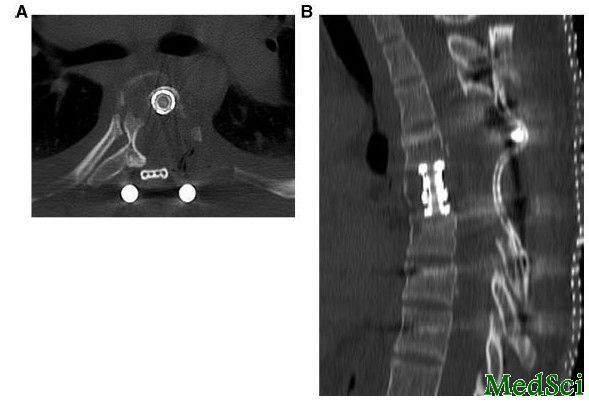
图1:A,CT显示mCT入路行T4椎体切除,近端肋骨和椎弓根切除,椎板和椎体切除。B,矢状位CT显示在切除椎体间隙内放置融合器。
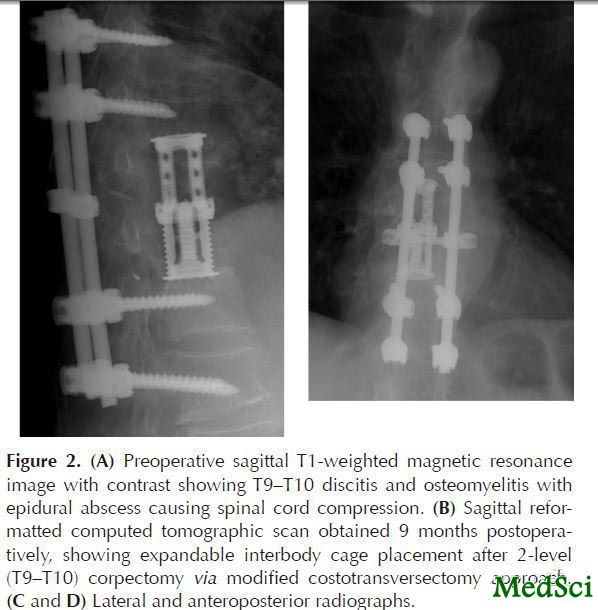
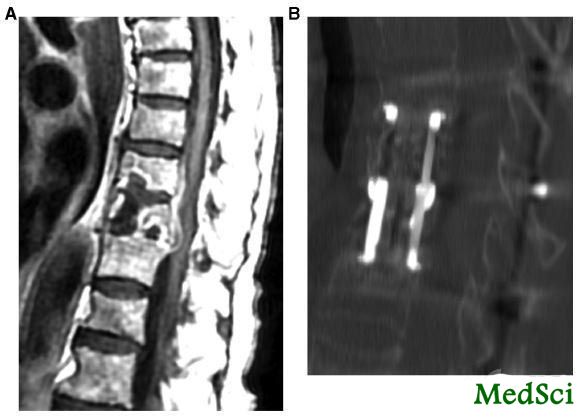
图2:A,术前MRI,T1增强相提示T9-T10节段骨髓炎+椎间盘炎,硬膜外脓肿出现脊髓压迫。B,术后9月矢状位重建CT显示2节段(T9-10)椎体切除术后可撑开椎间融合器位置。C-D,正位及侧位X片。
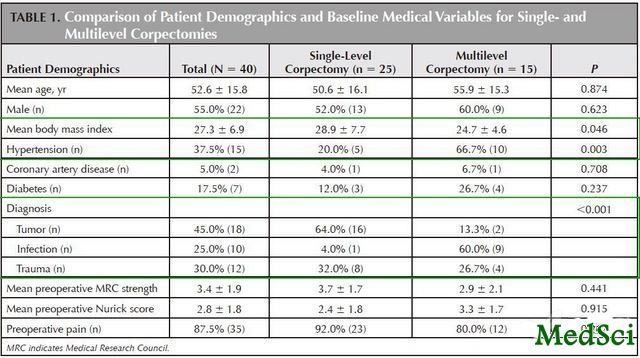
共40例患者符合研究纳入标准,平均年龄52.6岁,22例男性;18例肿瘤,10例感染,12例创伤。25例患者行单节段切除,15例患者行多节段切除(表1)。多节段切除患者中,2例3节段,其余为2节段。
表1所示人口统计学数据基线水平,大部分指标比较无显著差异(年龄 ( P = 0.874), 性别 ( P = 0.623), 冠心病 ( P = 0.708),),仅诊断类别,BMI,高血压等有所差异;术前肌力,MRC,Nurick评分,疼痛等均无显著差异。
表1:两组患者术前人口统计学数据比较
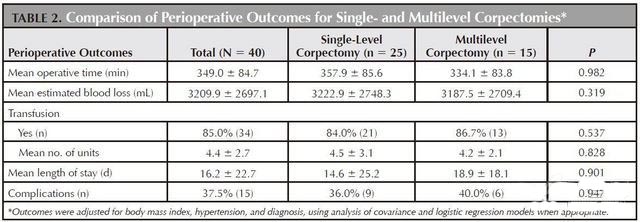
表2所示两组患者在术中及术后各项指标按BMI,高血压,诊断进行调整后的差异性对比。两组患者在手术时间(357.9 vs 334.1min,p=0.982),失血量(3222.9 vs3187.5ml,p=0.319),输血比例(84.0% vs 86.7%,p=0.537),输血量(4.5 vs 4.2u,p=0.828),平均住院日(14.6d vs 18.9d,p=0.901),并发症发生率(36% vs 40%,p=0.947,表3)等方面比较无显著差异。
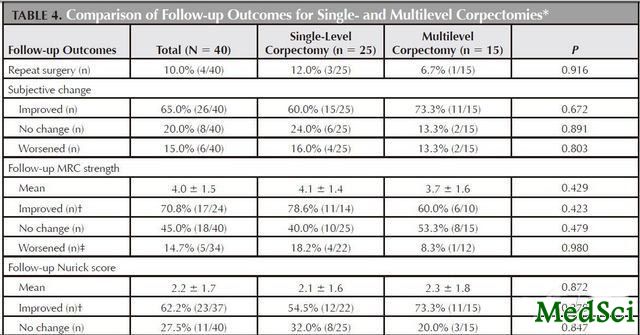
表4示两组患者术后再手术率和近期的随访结果。平均随访16.1月,3例患者死亡(2例为原有疾病进展,1例原因不详);总体再手术率10%,但组间比较无显著差异(12% vs 6.7%,p=0.916)。两组患者神经功能恢复和症状缓解(MRC,Nurick,疼痛等)无显著差异。
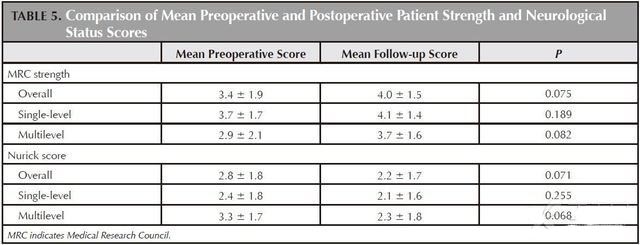
表5示术后两组患者MRC,Nurick,疼痛较术前改善情况,结果提示两者无显著差异(MRC改善 p=0.075,Nurick改善 p=0.071)。
表5:术后肌力,神经功能评分改善情况比较
研究者在文章最后讨论中对相关结果进行了分析:
1.本研究提示手术时间和手术切除节段无显著关系,这和我们传统的认知不同,具体的原因不详,但研究者认为可能和术者的手术经验,手术习惯,助手的配合程度,患者的一般情况,患者的疾病种类,脊柱稳定程度不同等相关;
2.患者术后住院时间组间比较无显著差异,但多节段组住院时间绝对值要显著大于单节段组,经过对患者人口统计学基线数据的调整后发现差别减少,提示住院时间差异可能是两组患者基线水平差异造成;
3.研究发现两组患者术后尽管存在较高的并发症发生率(40 %vs 36%),但组间比较无显著差异(p=0.947),和既往的文献报道的发生率(11.7-40%)相符合,提示后路多节段椎体切除技术可行,和单节段相比并不会显著增高并发症发生率。
4.术后对两组患者的随访中未发现有患者出现脊柱内固定的不稳定特征而需要再手术治疗;术后两组患者的功能评分无显著差异,功能改善尽管无显著差异,但多节段切除组在功能恢复趋势上更好,提示多节段椎体切除可能较单节段获益更多。
据此,研究者认为:改良后路经肋横突入路(mCT)行2个或以上节段切除椎体和单节段相比,无论是术中失血,手术时间和术后恢复,并发症发生率上均无显著差别,是一项行之有效的技术。
【编者按】几个问题:1.为何在T12,L1节段不能分离向外行走的神经根,其他节段可以?2.文中并没有提到所有患者是否由同一术者完成,这可能对手术结果造成重要影响,甚至是决定性的,这个结论是否可靠尚值得商榷。各位战友如何看待这个问题?

Perioperative characteristics, complications, and outcomes of single-level versus multilevel thoracic corpectomies via modified costotransversectomy approach.
STUDY DESIGN
Retrospective case series.
OBJECTIVE
To compare perioperative end points and outcomes of single-level versus multilevel corpectomy performed using a modified costotransversectomy approach.
SUMMARY OF BACKGROUND DATA
Single-level corpectomy via posterolateral approach has been shown to be an effective alternative to the traditional anterior thoracotomy approach. However, there is a paucity of studies that have examined multilevel thoracic corpectomy via posterolateral approach.
METHODS
Using electronic medical records, we identified a consecutive population of adult patients who underwent modified costotransversectomy corpectomy in the thoracic region between 2006 and 2009. Patients were stratified by number of corpectomies performed into either a single-level or multilevel group. With the use of baseline descriptive statistics and multivariate analysis, perioperative parameters and follow-up outcomes were assessed between the 2 groups.
RESULTS
A total of 40 patients were included in the final analysis, with 25 patients in the single-level group and 15 patients in the multilevel group. Mean follow-up was 16.1 months. Overall complication rate was 37.5%. Between the 2 groups, there were no significant differences in operative time, blood loss, transfusion rate, quantity of blood transfused, length of hospital stay, or complication rates. Also, there were no significant differences in repeat surgery rate, Medical Research Council strength, Nurick score, or pain at most recent follow-up, and all groups gained a comparable magnitude of benefit from surgery.
CONCLUSION
Multilevel corpectomy via modified costotransversectomy approach in the thoracic region is a feasible and effective option that does not seem to be associated with significantly increased morbidity. The degree of clinical improvement also seems comparable with single-level corpectomy.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Spine#
34
#切除术#
35
#椎体#
0