Circulation:炎症学说开创者Peter Libby提出精准诊疗急性冠脉综合征:根据炎症和影像学可分四种类型
2017-09-25 文韬 中国循环杂志
动脉粥样硬化炎症学说的开创者Peter Libby最近在Circualtion杂志发表了一篇重要文章。
动脉粥样硬化炎症学说的开创者Peter Libby最近在Circualtion杂志发表了一篇重要文章。
并据此将急性冠状动脉综合征分为四种类型:(1)炎症斑块破裂型;(2)无炎症斑块破裂型;(3)斑块侵蚀型;(4)痉挛和微血管病变型。
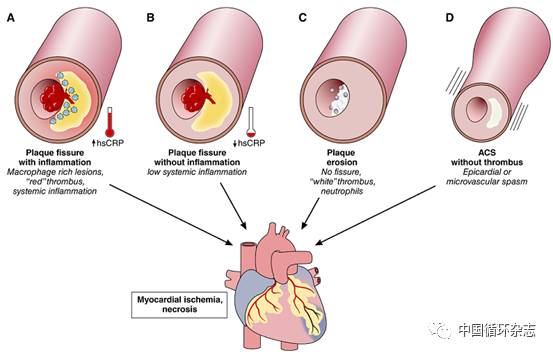
图1 Peter Libby提出的急性冠状动脉综合征的四种机制
A. 斑块破裂伴有局部炎症,血C反应蛋白升高
B. 有些患者的斑块破裂没有大量的炎症细胞聚集,没有血C反应蛋白升高
D. 痉挛和微血管病变也可导致急性冠状动脉综合征
Libby认为,指出目前临床治疗急性冠脉综合征主要是根据ST段是否抬高,但这已经是上个世纪的观点了。
而我们对急性冠状动脉综合征的临床、病理、细胞和分子层面认识的深入,尤其是影像学研究对急性冠脉综合征的机制已经有了进一步的认识。
他指出,仅仅根据斑块破裂来理解急性冠脉综合征太过简单,而忽略了许多基于其他机制的重要策略。
一、炎症型斑块破裂急性冠脉综合征证据最充分
Peter Libby提出了基于伴或不伴炎的斑块破裂导致的冠脉血栓。这一区分对抗炎治疗有重大意义。
关于炎症与心血管病,虽然Lippy的概念提出得很早,但一直没有证据,在最近欧洲心脏病学会(ESC)年会上公布并同步发表于《新英格兰医学杂志》的CANTOS研究显示,IL-1β单克隆抗体卡纳单抗可以在标准药物治疗基础上,将C反应蛋白>2 mg/dl、有心肌梗死病史者的心血管事件发生风险进一步降低15%,首次直接证明抗炎药物可以减少心血管疾病的发病。
二、非炎症斑块破裂型:或与胆固醇结晶形成有关
没有炎症的斑块破裂包括:体力活动或管壁局部张力增加,使斑块破裂;也包括地震或因喜欢的球队输球时心情不爽,导致了斑块破裂。这种类型的患者可能与交感神经兴奋或儿茶酚胺释放有关。
这种类型的急性冠脉综合征也是目前研究比较少。主要机制可能与脂核中胆固醇结晶形成有关,这种结晶的形成增加了斑块破裂和血栓形成的危险。

图2 胆固醇结晶形成的可能机制
三、斑块侵蚀型或可免于支架治疗
在强化降脂世代,斑块侵蚀导致的冠脉斑块破裂血栓形成正在增加。而识别斑块侵蚀导致急性冠脉综合征患者可使更多的患者免于有创治疗。
另外,对于用OCT识别出来斑块侵蚀型的急性冠状动脉综合征,有80%的血栓在1月时体积缩小50%,还有三分之一已经找不到血栓了,这些患者可能不需要置入支架。
由于他汀主要是通过降低低密度脂蛋白胆固醇(LDL-C)发挥作用,因此在他汀时代,如何针对富含甘油三酯的脂质组分减轻剩余风险,就有用武之地。
四、痉挛和微血管病变型血管性冠脉综合征:传统药物治疗还需加强
我们也认识到,急性冠脉综合征可以在没有明确的冠状动脉血栓或狭窄时发生,比如痉挛、微血管疾病等等,此类患者需要采取特定的策略,也应该有个性化和方式来处理。
在CASPAR研究中,有30%怀疑急性冠状动脉综合征的患者没有发现有罪犯病变。而有50%的患者在给予乙酰胆碱后诱发出了痉挛。
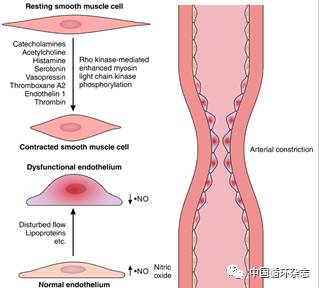
图3 血管痉挛的机制
微血管痉挛也可心肌缺血,这可见于应激型心肌病,15%有冠脉狭窄的患者也可存在微血管痉挛。
冠状动脉造影正常的患者中也可发生微血管痉挛。微血管痉挛可表现为心绞痛或非ST段抬高的心肌梗死,或使内皮损伤,导致斑块不稳定。
目前治疗上常用硝酸酯类和钙拮抗剂类药物治疗冠脉痉挛和微血管心绞痛,但还有很多患者症状不能缓解,有必要对冠脉平滑肌细胞的高反应性进一步研究。
原始出处:
Crea F, Libby P. Acute Coronary Syndromes: The Way Forward From Mechanisms to Precision Treatment. Circulation. 2017;136(12):1155-1166.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#PE#
20
#精准诊疗#
29
#PET#
31
#精准#
25
#综合征#
26
学习了
73
学习了.涨知识
75