Cell Research:孙颖浩发现中国人群前列腺癌特异融合基因
2012-04-10 孙颖浩等 Cell Research
孙颖浩教授 前列腺癌发病率在西方国家位于男性恶性肿瘤首位,随着我国社会人口老龄化,该病发病率近年来显著上升。前列腺癌有着明显的种族特异性,然而,产生这种特异性的分子生物学机制至今未明。 第二军医大学长海医院孙颖浩教授运用RNA-seq技术首次对中国人前列腺癌及癌旁组织进行系统研究,发现新型融合基因、癌相关长链非编码RNA、异构体和点突变。研究发现,在欧美人群中普遍高频表达(50-80%)的融合

孙颖浩教授
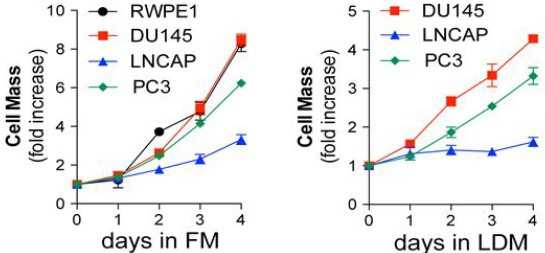
前列腺癌发病率在西方国家位于男性恶性肿瘤首位,随着我国社会人口老龄化,该病发病率近年来显著上升。前列腺癌有着明显的种族特异性,然而,产生这种特异性的分子生物学机制至今未明。
第二军医大学长海医院孙颖浩教授运用RNA-seq技术首次对中国人前列腺癌及癌旁组织进行系统研究,发现新型融合基因、癌相关长链非编码RNA、异构体和点突变。研究发现,在欧美人群中普遍高频表达(50-80%)的融合基因TMPRSS2-ERG在中国人群中的表达率仅有20%左右,而在欧美人群中尚未发现的融合基因CTAGE5-KHDRBS3和USP9Y-TTTY15在中国人群中却有很高的表达频率,分别为37%和35.2%,提示这些融合基因具有中国人群特异性。相关论文发表在2月21日的《细胞研究》(Cell Research)杂志上。
研究人员发现多个癌组织差异性表达的长链非编码RNA进行了验证,发现PCA3,FR0348383 和 MALAT-1在癌组织中的过表达率分别为80%,72.5%和82.5%,FR0257520 在癌组织中的低表达率为82.5%。此外,研究者还发现并验证了PSA新型异构体,具有潜在的诊断价值。
研究人员根据此次研究结果绘制了中国人群特异性的前列腺癌图谱,提出了3条关键信号通路,为深入认识中国人群前列腺癌的发生发展机制奠定基础。这些研究成果是第二代测序的成功范例,首次揭示了中国人群前列腺癌的全貌,新研究为进一步了解前列腺癌的诊断、发病演化机制和种族差异性提供了新线索。(生物谷 bioon.com)

doi:10.1038/cr.2012.30
PMC:
PMID:
RNA-seq analysis of prostate cancer in the Chinese population identifies recurrent gene fusions, cancer-associated long noncoding RNAs and aberrant alternative splicings
Shancheng Ren, Zhiyu Peng, Jian-Hua Mao, Yongwei Yu, Changjun Yin, Xin Gao, Zilian Cui, Jibin Zhang, Kang Yi, Weidong Xu, Chao Chen, Fubo Wang, Xinwu Guo, Ji Lu, Jun Yang, Min Wei, Zhijian Tian, Yinghui Guan, Liang Tang, Chuanliang Xu, Linhui Wang, Xu Gao, Wei Tian, Jian Wang, Huanming Yang, Jun Wang and Yinghao Sun
There are remarkable disparities among patients of different races with prostate cancer; however, the mechanism underlying this difference remains unclear. Here, we present a comprehensive landscape of the transcriptome profiles of 14 primary prostate cancers and their paired normal counterparts from the Chinese population using RNA-seq, revealing tremendous diversity across prostate cancer transcriptomes with respect to gene fusions, long noncoding RNAs (long ncRNA), alternative splicing and somatic mutations. Three of the 14 tumors (21.4%) harbored a TMPRSS2-ERG fusion, and the low prevalence of this fusion in Chinese patients was further confirmed in an additional tumor set (10/54=18.5%). Notably, two novel gene fusions, CTAGE5-KHDRBS3 (20/54=37%) and USP9Y-TTTY15 (19/54=35.2%), occurred frequently in our patient cohort. Further systematic transcriptional profiling identified numerous long ncRNAs that were differentially expressed in the tumors. An analysis of the correlation between expression of long ncRNA and genes suggested that long ncRNAs may have functions beyond transcriptional regulation. This study yielded new insights into the pathogenesis of prostate cancer in the Chinese population.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#孙颖浩#
0
#Cell#
36
#CEL#
35
#融合#
40
#融合基因#
37
#Research#
35