Europace:不间断抗凝的AF消融患者仍有无症状性脑损伤风险
2013-03-13 Europace 丁香园
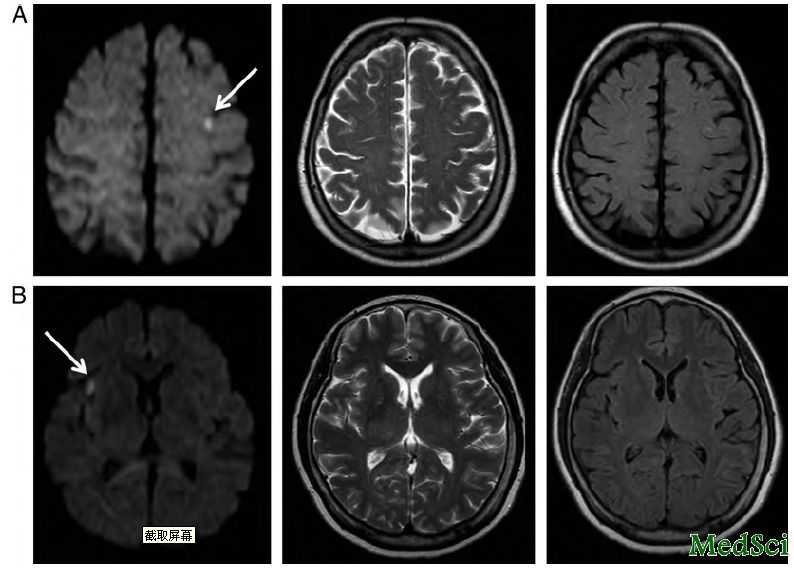
两例代表性急性脑栓塞 已经证实在左房的射频消融可导致无症状性脑损伤风险。目前尚无在不间断口服抗凝治疗的患者接受AF射频消融过程中发生脑损伤的资料。奥地利的研究人员Martin Martinek等开展的这项研究的目的旨在通过术前和术后核磁共振(MRI)对国际标准化比值(INR)治疗范围内的无症状性脑损伤患者发生情况进行量化来寻找与脑栓塞相关的临床或者手术影响因素。其结果发表在在2013年3月的
已经证实在左房的射频消融可导致无症状性脑损伤风险。目前尚无在不间断口服抗凝治疗的患者接受AF射频消融过程中发生脑损伤的资料。奥地利的研究人员Martin Martinek等开展的这项研究的目的旨在通过术前和术后核磁共振(MRI)对国际标准化比值(INR)治疗范围内的无症状性脑损伤患者发生情况进行量化来寻找与脑栓塞相关的临床或者手术影响因素。其结果发表在在2013年3月的Europace杂志上。
研究共纳入连续的131例接受导管射频消融的阵发性房颤患者(n=80,61.1%)或者持续性房颤患者(n=51,38.9%)。利用3.5mm开放式灌注导管根据具体情况行肺静脉前庭(PVI)、顶部线、二尖瓣峡部线、以及碎裂点位(CFAE)消融。所有的患者均接受术前和术后头颅MRI。术后MRI发现16例患者出现新的栓塞性病变(12.2%),但他们均无症状。在单因素分析中,临床资料中的年龄(P = 0.027)、持续性房颤(与阵发性AF对比;P = 0.039)、经食道超声心动图时自主回声增强(P = 0.029)与脑栓塞明显相关。有意义的术中影响因素有电复律(P = 0.041)、仅行PVI(P = 0.008)以及碎裂电位消融(P = 0.005)。多因素分析中,独立的危险因素为年龄(P = 0.009)、自主回声增强(P = 0.029)和 CFAE消融(P = 0.006)。
不间断口服抗凝治疗的房颤患者接受射频消融术仍有较大的无症状脑栓塞风险(头颅MRI检查发现)。因此,持续口服抗凝不能预防脑栓塞发生。多种不同的临床和手术因素共同导致脑损伤风险。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#间断#
30
#ACE#
27
#损伤#
37
#消融#
32
#无症状#
43