Gastroenterology:新发糖尿病患者胰腺导管腺癌筛查有新方法啦!
2016-12-12 xing.T MedSci原创
研究者开发了一个基于广泛使用的临床参数的风险模型来帮助确定新发糖尿病患者中可以从PDA筛选中受益的个体。
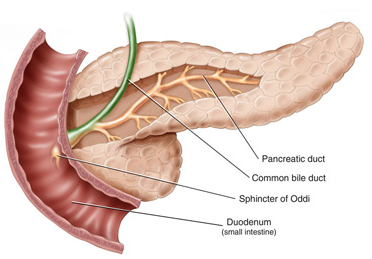
大约50%的胰腺导管腺癌(PDA)患者在肿瘤诊断之前就诊断出糖尿病。对新发糖尿病的个体进行筛选可能现实对PDA的早期诊断。近日,消化病领域顶级杂志Gastroenterology上发表了一篇研究文章,该研究旨在开发和验证一个PDA的风险预测模型来识别新发糖尿病患者中的高风险个体。
研究人员在英国具有人群代表性的数据库中进行了一项回顾性队列研究。研究者纳入了35岁以下的新发糖尿病患者,并且在诊断后对这些患者进行3年以上的随访。在糖尿病诊断时候选预测因子包括流行病学和临床特征。在单因素分析中P值小于25的变量采用向后逐步分析法进一步评估。使用受试者工作特征曲线分析对模型的辨别度进行了评估。采用Hosmer-Lemeshow检验进行校准,使用引导程序对研究结果进行内部验证。
研究人员分析了109,385例新发糖尿病患者的数据。其中,有390例(0.4%)在3年内被诊断患有PDA。最终的模型(曲线下面积为0.82;95%可信区间为0.75–0.89)包括年龄、体重指数、体重指数变化值、吸烟、使用质子泵抑制剂和抗糖尿病药物、糖化血红蛋白、胆固醇、血红蛋白、血肌酐和碱性磷酸酶。引导(程序)证实显示只有微不足道的好处。如果3年间PDA筛选设定的预测风险阈值为1%,只有6.19%的新发糖尿病人口将进行最终的筛选,从而确诊PDA患者的敏感性为44.7%、特异性为94%以及阳性预测值为2.6%。
由此可见,研究者开发了一个基于广泛使用的临床参数的风险模型来帮助确定新发糖尿病患者中可以从PDA筛选中受益的个体。
原始出处:
Ben Boursi, et al. A Clinical Prediction Model to Assess Risk for Pancreatic Cancer Among Patients With New-onset Diabetes. Gastroenterology .2016.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#GAS#
38
#Gastroenterol#
34
#AST#
29
#新方法#
37
很好,不错,以后会多学习
66
很好,不错,以后会多学习
73
#糖尿病患者#
24
#Gastroenterology#
25