高血压是脑卒中的主要危险因素,是美国女性死亡的第三大原因,男性死亡的第五大原因。高血压被认为是首次或复发中风的最重要的危险因素。如果高血压得到治疗和控制,中风基本上是可以预防的。
许多随机对照试验表明,降低血压(BP)可以减少中风的风险。与白人成年人相比,普通人群中的黑人成年人控制血压的可能性较低。
2014年美国心脏协会(AHA)/美国卒中协会指南建议,对于以前接受过治疗的神经系统稳定者,在急性卒中后恢复降压药物治疗,对于收缩压(SBP)≥140毫米汞柱或舒张压(DBP)≥90毫米汞柱者启动降压药物治疗。
与以前的指南相比,2017年美国心脏病学院(ACC)/AHA血压指南为有中风史的成年人设定了较低的血压目标,即SBP/DBP<130/80 mm Hg。
很少有研究使用2017年ACC/AHA血压指南的阈值来评估卒中幸存者中血压控制的种族差异。
藉此,University of Alabama的Oluwasegun P. Akinyelure等人,利用2017年ACC/AHA血压指南的阈值来研究中风后血压控制的种族差异。
为了进行比较,他们还研究了未发生中风的参与者在血压控制方面的种族差异。为了实现这些目标,他们分析了REGARDS(Reasons for Geographic and Racial Differences in Stroke )研究的数据。并假设,与有或无中风史的白人成年人相比,黑人控制血压的可能性较低。
他们研究了在基线(2003-2007年)和第二次随访(2013-2016年)期间服用抗高血压药物的参与者,他们是否经历过中风(分别为306人和7693人)。
第二次随访时的血压控制被定义为收缩压<130毫米汞柱和舒张压<80毫米汞柱,但年龄≥65岁的低风险成人(即没有糖尿病、慢性肾病、心血管疾病史,且10年预测动脉粥样硬化性心血管疾病风险<10%的人)除外,他们的血压控制被定义为收缩压<130毫米汞柱。
在有中风史的参与者中,50.3%的白人参与者控制了血压,而黑人参与者为39.3%。在没有中风史的参与者中,56.0%的白人参与者控制了血压,而黑人参与者为50.2%。
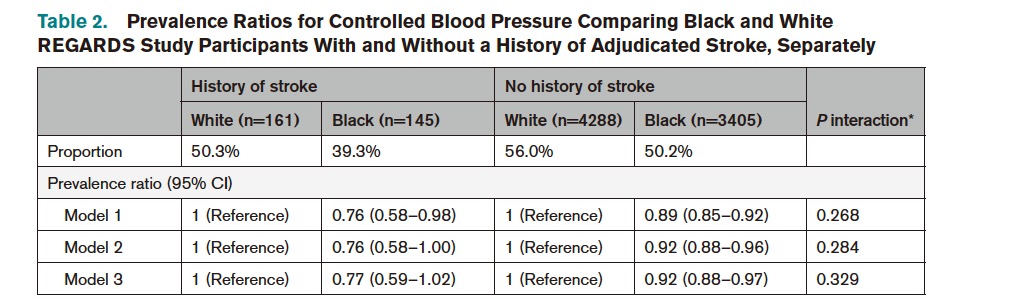 经过多变量调整后,黑人参与者比白人参与者更不可能控制血压(有中风史的参与者的流行率为0.77[95%CI,0.59-1.02],无中风史的参与者为0.92[95%CI,0.88-0.97])。
经过多变量调整后,黑人参与者比白人参与者更不可能控制血压(有中风史的参与者的流行率为0.77[95%CI,0.59-1.02],无中风史的参与者为0.92[95%CI,0.88-0.97])。
这个研究的重要意义在于发现了:与有或无卒中的白人成年人相比,黑人控制血压的比例较低,经多变量调整后无统计学意义的差异。
原文出处:
Akinyelure OP, Jaeger BC, Moore TL, et al. Racial Differences in Blood Pressure Control Following Stroke: The REGARDS Study. Stroke. Published online September 2, 2021. doi:10.1161/STROKEAHA.120.033108
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#血压管理#
49
#种族差异#
37
已学
61
学习
60
学习
64
已了解
64
中风是俗称,应该称为缺血性卒中吧
53