NEJM:食管贲门失弛缓症-案例报道
2015-12-17 chenshuo译 MedSci原创
男性,63岁,既往有甲状腺功能减退病史,今因出现吞咽困难(固体食物或流质)10余年来未来院就诊。
男性,63岁,既往有甲状腺功能减退病史,今因出现吞咽困难(固体食物或流质)10余年来未来院就诊。
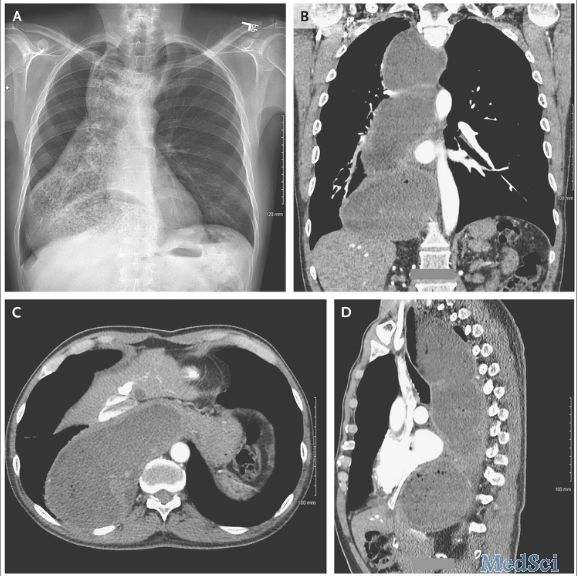
胸部X线检查结果如图A所示(患者直立体位内部纵隔结构)。
CT成像扫描显示近端食管至胃食管交界处(图B为冠状面扫描,图C为截面视图,图D为矢状面扫描)。
胃镜检查显示食管内大量食物潴留并伴有明显地食管扩张,但未发现有狭窄或肿块的迹象。
根据该患者的临床症状及检查结果,会诊医师诊断其为食管贲门失弛缓症。
食管贲门失弛缓症一般是由食管下括约肌松弛受损引起的,最常见的临床症状为吞咽固体食物和流质食物出现困难。
针对该患者的情况,主治医生决定对其进行手术治疗并放置空肠营养管给予肠内营养支持。8个月后,该患者恢复良好,逐步开始自行进食,不久随即拔出空肠营养管。
Chinemerem Okwara, M.D,and David Cangemi, M.D.Achalasia with Megaesophagus.NEJM.2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#贲门#
31
是一篇不错的文章
114
值得进一步关注
155
不错,赞一个
107
这篇文章有一定深度
108
#食管贲门失弛缓症#
31
吓到了
116
赞?
46
好文章,值得看。
74
赞
42