超级耐药菌克星问世:科学家发现新抗生素
2015-01-12 佚名 腾讯科技
科学家已经发现了一种与现存抗生素同样有效的新型抗生素,这一发现也是近30年来的首次。实验室测试已经表明,这种名为teixobactin的新抗生素杀死某些细菌的速度与现存抗生素的速度相当,而且能够在无毒副作用的情况下治愈实验鼠的细菌感染。 研究同样表明,原型药物对抗有害菌的方式完全不同,不太可能引发耐药性,这也是研发新抗生素的最大阻碍。去年就有研究人员发出警告称,医药行业可能会退回到黑暗时代
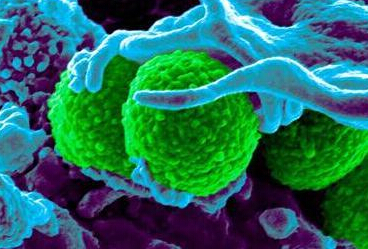
科学家已经发现了一种与现存抗生素同样有效的新型抗生素,这一发现也是近30年来的首次。实验室测试已经表明,这种名为teixobactin的新抗生素杀死某些细菌的速度与现存抗生素的速度相当,而且能够在无毒副作用的情况下治愈实验鼠的细菌感染。
研究同样表明,原型药物对抗有害菌的方式完全不同,不太可能引发耐药性,这也是研发新抗生素的最大阻碍。去年就有研究人员发出警告称,医药行业可能会退回到黑暗时代,人们有可能因为缺乏有效的抗生素死于不太严重的感染。由于超级细菌耐药性及其全球传播的快速增长,有效的抗生素正越来越少,而这一发现将代表着医药领域的巨大进步。
这项研究的负责人,东北大学的Kim Lewis教授称:“首次人类临床试验将在两年内开始,如果试验成功,这种药物有可能在10年内广泛使用。病原体获得抗药性的速度远快于我们研发新抗生素的速度,这会导致人类健康出现危机。我们已经发现部分肺结核病菌对全部抗生素都有抗性。Teixobactin对于肺结核非常有效,而且有可能形成一种只依靠Teixobactin的单药物疗法。”
Lewis教授称:“细菌通过蛋白质变化形成抗药性,teixobactin的目标并非蛋白质,而是细胞被组建模块的聚合物前驱体。”欧洲每年约有2.5万人因抗生素治疗无效而死于感染,世界卫生组织将耐药性描述为现代医学面临的最显著全球风险之一。爱丁堡大学传染病学的Mark Woolhouse博士称:“新抗生素的任何报告都是喜人的,而最让我激动的是这项研究的发现仅仅揭开了冰山一角。”
但是帝国理工学院的Angelika Gründling博士读完这篇论文后称:“我们需要记住的是,新抗生素目前只对某些细菌有效。论文中描述的新抗生素尚未在人类身上进行测试,有可能它并非像我们期盼中的那样有效,而且也可能存在未知的副作用限制它的使用。”
原始出处:
Heidi Ledford. Promising antibiotic discovered in microbial 'dark matter'. Nature
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#科学家发现#
28
#耐药菌#
36
hao
118
Haida
107
好内容!
88