Front Oncol:回顾性分析伊立替康治疗既往接受过蒽环类和紫杉类药物的转移性乳腺癌患者的疗效
2021-11-22 yd2015 MedSci原创
研究表明,对于既往使用蒽环类和/或紫杉类药物治疗的MBC患者,含伊立替康方案获得了中等的客观反应,并有生存获益的趋势,值得进一步研究。
目前,转移性乳腺癌(MBC)患者在接受蒽环类和紫杉类药物治疗进展后,治疗选择的药物较少。有研究表明,伊立替康对一些以前使用过蒽环类药物和紫杉类药物的患者具有中等强度的抗肿瘤活性。近期,Frontiers in Oncology杂志上发表了来自四川大学华西医院团队的一项研究结果,旨在评估以伊立替康为基础的化疗对转移性乳腺癌患者的疗效。
研究回顾性性收集四川大学华西医院51例接受伊立替康治疗的MBC患者的临床资料和生存资料。主要研究终点为无进展生存期(PFS)和总生存期(OS),次要终点为客观缓解率(ORR)。为了最小化降低潜在混淆因素的影响,研究通过基于年龄、激素受体(HR)和人表皮生长因子受体2 (HER2)等因素进行倾向评分匹配(PSM),对51名接受三线化疗但未接受伊立替康的患者进行匹配,并将其OS和PFS与接受伊立替康治疗的患者进行比较。
51例患者中,中位年龄为43岁,绝经前患者占60%以上。生物亚型包括雌激素受体(ER)阳性和/或孕激素受体(PR)阳性(74.5%),HER2阳性(35.3%)和三阴性(13.7%)。超过85%的患者发生内脏转移,超过85%的患者曾接受过蒽环类药物治疗,超过95%的患者曾接受过紫杉烷类药物治疗。既往中位治疗线数为4,中位化疗周期数为2周期(范围1-14周期)。
截止2020年10月30日,伊立替康组的最佳总体缓解为:CR (n =1)、PR (n =7)、SD (n = 11)、进展性疾病(PD) (n = 32), ORR为15.7%,DCR为37.3%。伊立替康组的中位PFS为3.2个月(95% CI 2.7 3.7)。PSM后,伊立替康组较非伊立替康组在数值上延长PFS,分别为3.2个月(95% CI 2.7 3.7)和2.1个月(95% CI 1.4 2.8),但无统计学意义(P = 0.052)。
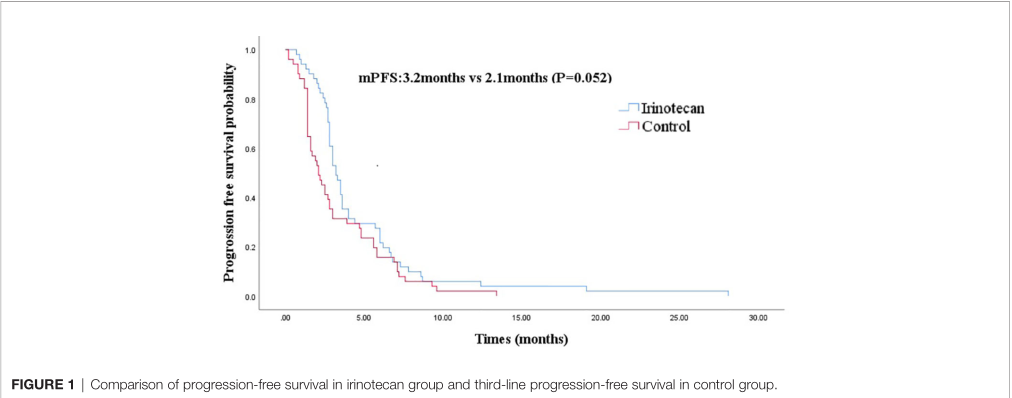
PFS
患者中位OS为33.1个月(95% CI 27.9 38.3), 2年OS率为70.0%。PSM后,伊立替康组较非伊立替康组在数值上延长OS,分别为33.1个月(95% CI 27.4–38.8)和18.0个月(95% CI 3.2–32.8),但无统计学意义(P = 0.072)。
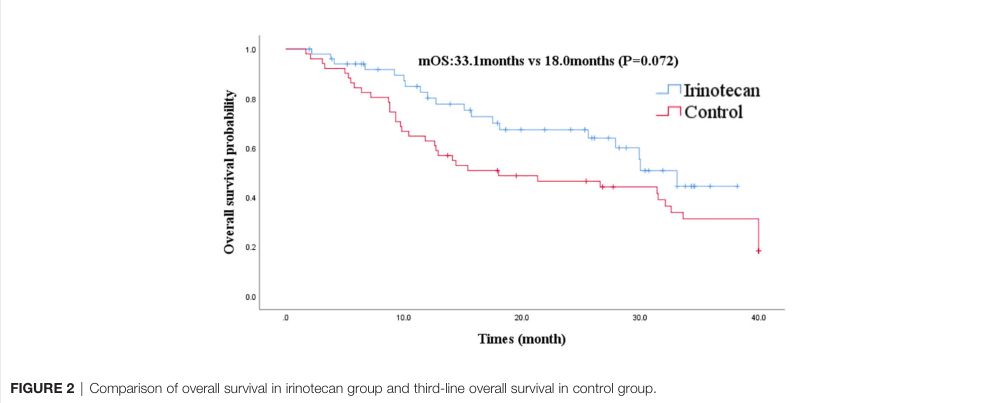
OS
单因素分析结果显示,与未发生内脏转移的患者相比,发生内脏转移患者使用伊立替康的PFS明显延长(P = 0.031)。年龄(<45岁,≥45岁),绝经状态(绝经前,绝经后),三阴性(阳性/阴性),HER2状态(阳性/阴性),HR状态(阳性/阴性),以及既往化疗线数(≤3,>3)与伊立替康治疗的PFS无关。单因素分析未发现影响OS的临床病理因素。
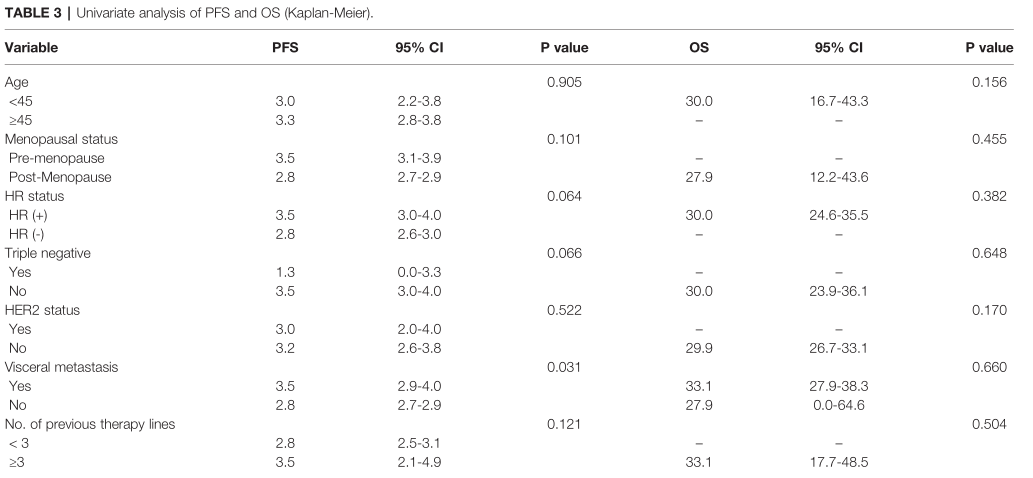
单因素分析PFS和OS
亚组分析发现,小于45岁(P=0.039)、绝经前(P=0.004)、HR阳性(P=0.021)、非三阴性(P=0.039)、有脏器转移(P= 0.028)、既往接受过蒽环类药物治疗(P=0.025)的患者使用伊立替康治疗时PFS更长。使用伊立替康治疗的绝经前患者(P=0.029) 有较长的OS。其他因素未发现与患者PFS和OS显著相关。
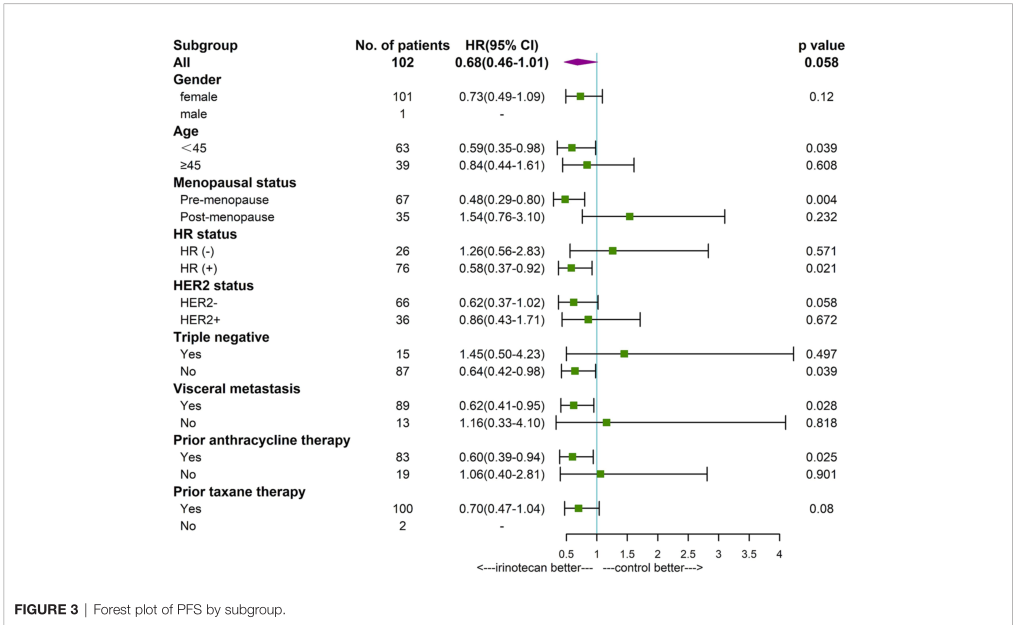
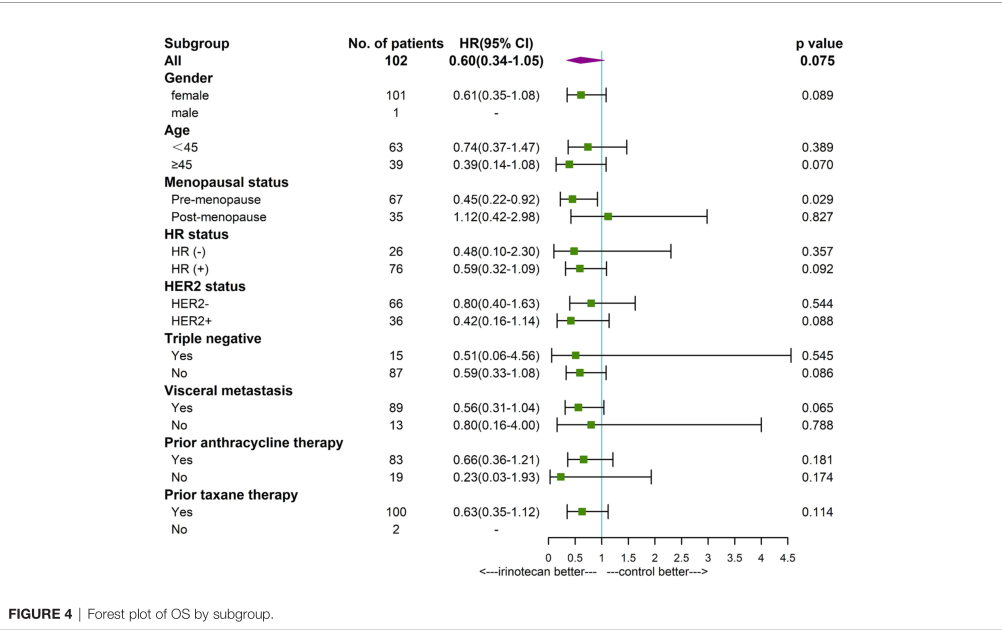
PFS和OS的亚组分析
绝大多数患者在伊立替康治疗进展后接受进一步治疗:52例(86.7%)患者接受了全身治疗。由于接受后续治疗的患者比例较高,必然会影响OS, 2年OS率等指标可能更可靠地反映伊立替康治疗MBC患者的疗效。
综上,研究表明,对于既往使用蒽环类和/或紫杉类药物治疗的MBC患者,含伊立替康方案获得了中等的客观反应,并有生存获益的趋势,值得进一步研究。
原始出处:
Suo J, Zhong X, He P, Zheng H, Tian T, Yan X and Luo T (2021) A Retrospective Analysis of the Effect of Irinotecan-Based Regimens in Patients With Metastatic Breast Cancer Previously Treated With Anthracyclines and Taxanes. Front. Oncol. 11:654974. doi: 10.3389/fonc.2021.654974
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncol#
0
#转移性#
39
#回顾性分析#
52
#蒽环类#
44
#紫杉类药物#
54
#乳腺癌患者#
42
学到了
70