Injury:早期软组织覆盖和VSD可以改善下肢严重创伤结局
2012-08-13 紫川秀第二 丁香园
对下肢软组织创伤合并骨折病人而言,内固定取得骨折部位稳定后进行软组织覆盖可以有效地改善患者的下肢功能预后。而软组织重建的时间点目前争议很大,24小时,3天,1周等时间点均有报道,而对于金属内固定物而言,无软组织覆盖暴露在空气中会产生较多的并发症,因此需要及时地软组织覆盖,有报道使用真空的负压吸引装置(VSD)进行污染创面的临时覆盖可以减少组织水肿,促进肉芽组织
对下肢软组织创伤合并骨折病人而言,内固定取得骨折部位稳定后进行软组织覆盖可以有效地改善患者的下肢功能预后。而软组织重建的时间点目前争议很大,24小时,3天,1周等时间点均有报道,而对于金属内固定物而言,无软组织覆盖暴露在空气中会产生较多的并发症,因此需要及时地软组织覆盖,有报道使用真空的负压吸引装置(VSD)进行污染创面的临时覆盖可以减少组织水肿,促进肉芽组织生长,但VSD装置能不能减少的使用在延长创面暴露时间时是否会增加相关并发症目前并无报道。来自澳大利亚的学者近期就自由软组织皮瓣重建修复创面及VSD应用等相关问题进行了系统性研究,评估了延迟软组织重建,延长金属内固定物暴露,皮瓣移植前创面感染,VSD应用等因素对患者预后的影响,相关结论发表在近期出版的injury上。
研究者选取2002年7月至2009年6月间在Royal Melbourne Hospital就诊的患者,共103名,共105处创面进行游离皮瓣重建。获取的研究数据包括:病人的一般情况,创伤机制,ISS评分,开放骨折的GA分级,ASA评分,受伤地点,接受治疗的时间,软组织重建的时间,金属内固定物暴露的时间,皮瓣移植时创面感染情况,是否适用VSD,手术治疗的内固定方法,游离皮瓣的获取部位,术后1年患者的预后,并发症及转移皮瓣的状况等(表1,2)。内固定和皮瓣转移预后的评价主要指标包括:皮瓣的take-backs,皮瓣缺失,深部金属内固定物感染,骨髓炎,影像学不愈合,术后1年患肢的负重情况等;而次要指标包括:住院周期(length of stay,LOS),手术时间,总体手术治疗次数,游离皮瓣移植后的手术治疗次数。
研究结果提示:和三天内进行游离皮瓣重建的患者相比,延迟至七天后重建的患者,在重建前创面感染率,皮瓣再次手术,深部金属内固定物感染,骨髓炎等发生方面显着增高(表3,图1);皮瓣重建前的创面感染可以作为患者预后较差的一个预测指标;而在金属内固定物暴露组别,若内固定物暴露超过1天后进行游离皮瓣的重建会显着增加失败的风险,并且会显着延长住院周期(表4);对使用真空负压吸引装置的创面可以减少手术次数和深静脉血栓发生机率,但在延长创面暴露时间从而降低术后并发症方面并没有实际效果。
表1:延迟游离皮瓣重建和创面预后的关系
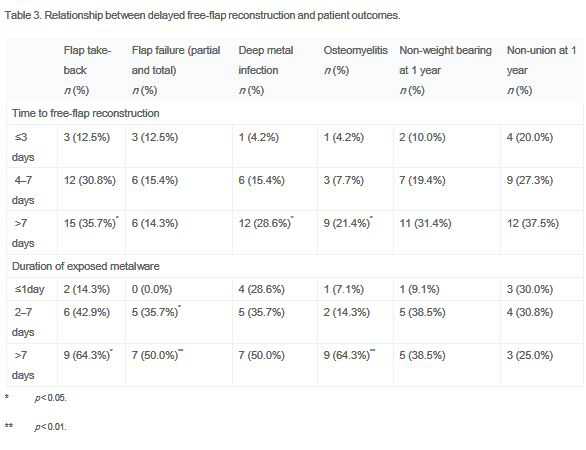
表2:延迟游离皮瓣重建和住院周期的关系
图1:游离皮瓣重建时间点和并发症的关系
图2:游离皮瓣重建时间点,金属内固定物暴露时间点和重建前创面感染的关系
表3:游离皮瓣重建前创面感染对皮瓣重建结果的影响(多因素分析后结果)
作者总结:1,3天内进行软组织缺损的游离皮瓣重建可使患者获得较好的预后,而创面暴露超过7天意味着并发症明显增加;2,一旦金属内固定物暴露,无软组织覆盖,应当立即进行软组织覆盖重建;延迟一天进行覆盖会造成严重并发症;3.VSD可以减少皮瓣的take-backs机会,但也会增加皮瓣的失败,感染,骨髓炎等的机会,并且应用VSD时将创面覆盖时间延迟至7天后并不会显着降低创面覆盖后的并发症;所以对开放性创伤的患者而言,及时地软组织覆盖,有效地抗生素应用等可以减少并发症的发生,所以在处理时的原则是及时、有效!
原文链接:
Liu DS, Sofiadellis F, Ashton M, MacGill K, Webb A. Early soft tissue coverage and negative pressure wound therapy optimises patient outcomes in lower limb trauma. Injury. 2012 Jun;43(6):772-8.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#严重创伤#
29
#VSD#
37
#Injury#
32
#创伤#
29
#软组织#
29