Sci Signal:维生素C为何可能降低神经退行性疾病风险?
2017-04-08 佚名 学术经纬
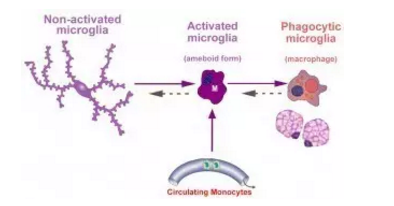
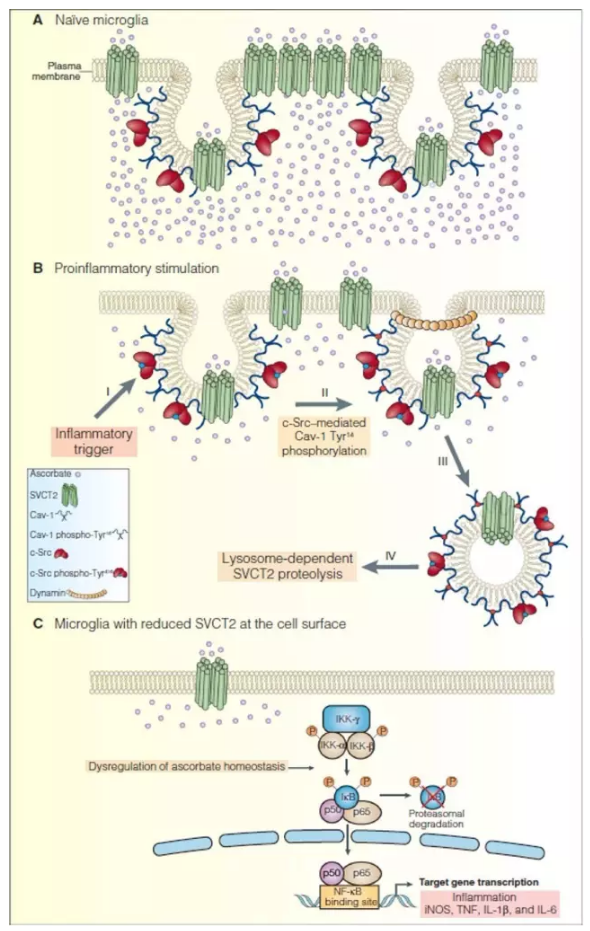
最近,葡萄牙波尔图大学(Universidade do Porto)的研究人员发现了维生素C对大脑的另一项重要意义,那就是防止出现过度的炎症反应。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#退行性疾病#
46
#Signal#
30
#Sign#
40
#神经退行#
39
#疾病风险#
35