Front Cardiovasc Med:保留射血分数的心力衰竭患者转用沙库巴曲/缬沙坦后降低肺动脉高压
2021-11-09 刘少飞 MedSci原创
由于伴有肺动脉高压的 HFpEF 患者表现出特别高的死亡率和发病率,我们评估了沙库巴曲/缬沙坦在该 HFpEF 患者亚组中的作用。

射血分数保留的心力衰竭 (HFpEF) 是目前最常见的心力衰竭形式,其发病率在全球范围内仍在继续增长,但仍没有获得批准的指南治疗。就在最近,PARAGON-HF 试验未能揭示沙库巴曲/缬沙坦在 HFpEF 患者中使用沙库巴曲/缬沙坦抑制血管紧张素受体 - 脑啡肽酶在其主要复合结局(心力衰竭住院治疗和心血管原因死亡)方面的显着益处。尽管如此,该试验提供了重要的意义,因为预先指定的患者亚组被确定为仍可能受益于沙库巴曲/缬沙坦治疗。Solomon 等人概述的女性和射血分数或肾功能中度降低的患者显示出显着改善的主要结果。
在肺动脉高压大鼠模型中,沙库巴曲/缬沙坦已被证明可降低肺压和组织学血管重构,其他研究表明,沙库巴曲/缬沙坦可降低射血分数降低的心力衰竭 (HFrEF) 患者的肺压。合并肺动脉高压的 HFpEF 患者的长期死亡风险显着升高,并且就呼吸困难而言遭受的影响最大。
因此,我们试图调查沙库巴曲/缬沙坦是否会影响根据 HFA-PEFF 算法诊断出的其他异质性 HFpEF 患者亚组的肺动脉高压。
研究方法:
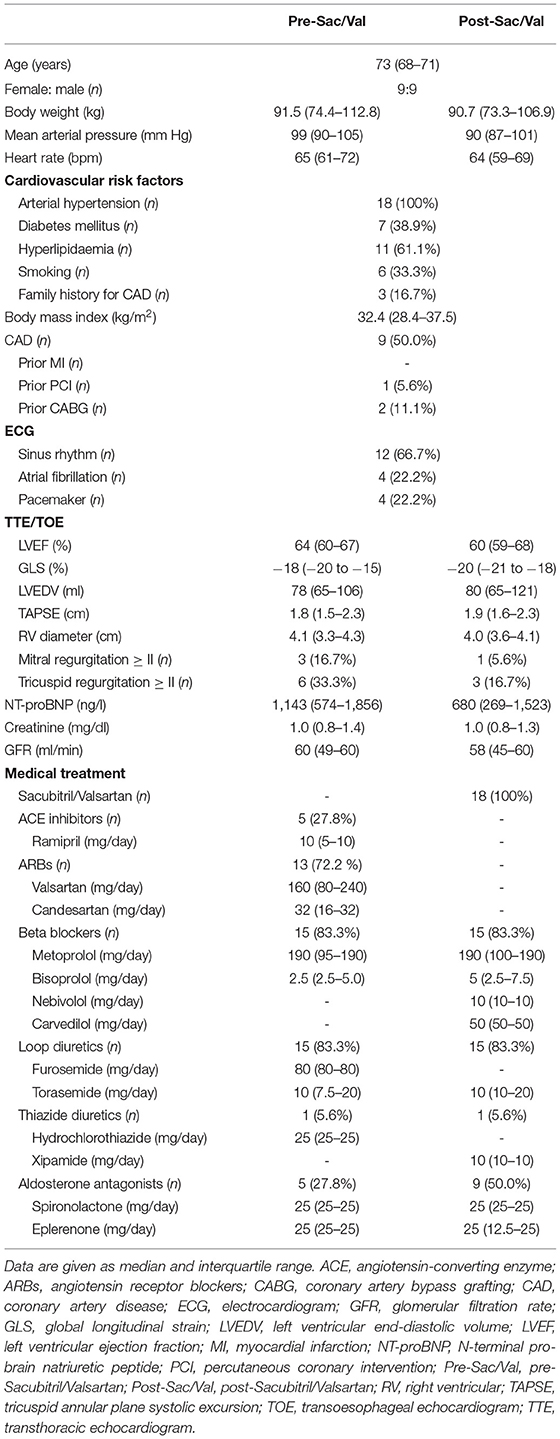
这是一项回顾性病例系列,纳入 18 名以 HFpEF 和呼吸困难为主要住院症状的患者(2018 年 1 月至 2020 年 8 月),在这些患者中,经主治医师酌情开始使用沙库巴曲/缬沙坦。在没有沙库巴曲/缬沙坦(前沙库巴曲/缬沙坦)的情况下,在基线时通过右心导管插入术 (RHC) 确定有创肺压。沙库巴曲/缬沙坦对肺压的影响在 99 (71–156) 天后,在计划的第二次入院和 RHC 随访期间(沙库巴曲/缬沙坦后)记录在案。
所有 RHC 均在导管插入实验室中使用飞利浦 Allura Xper FD10 心血管 X 射线系统进行,包括 Xper Flex 心脏生理监测系统,用于记录呼气末肺动脉压 (PAP)、平均肺毛细血管楔压 (PCWP)、右心房 ( RA) 压力和计算肺血管阻力 (PVR)、心输出量 (CO)、心脏指数 (CI) 和全身血管阻力 (SVR)。CO 根据 Fick 原理计算。Sacubitril/Valsartan RHC 前后均由同一位心脏病专家进行,使用 7F Swan-Ganz 导管经股静脉通路是首选方法。
研究结果:
转化为沙库巴曲/缬沙坦后,显示出RHC减压显著肺动脉压(PAP),并与预先沙库巴曲/缬沙坦[平均肺毛细血管楔压(PCWP)PAP收缩/舒张/平均44(38-55)/ 15 (11-20)/27 (23-33) 毫米汞柱与 51 (41-82)/22 (13-29)/33 (28-52) 毫米汞柱,p < 0.05 和p< 0.01,分别;PCWP 16 (12-20) 毫米汞柱与 22 (15-27) 毫米汞柱,p < 0.05]。中值沙库巴曲/缬沙坦剂量为 24/26 mg BID (24/26 BID-49/51 mg BID)。
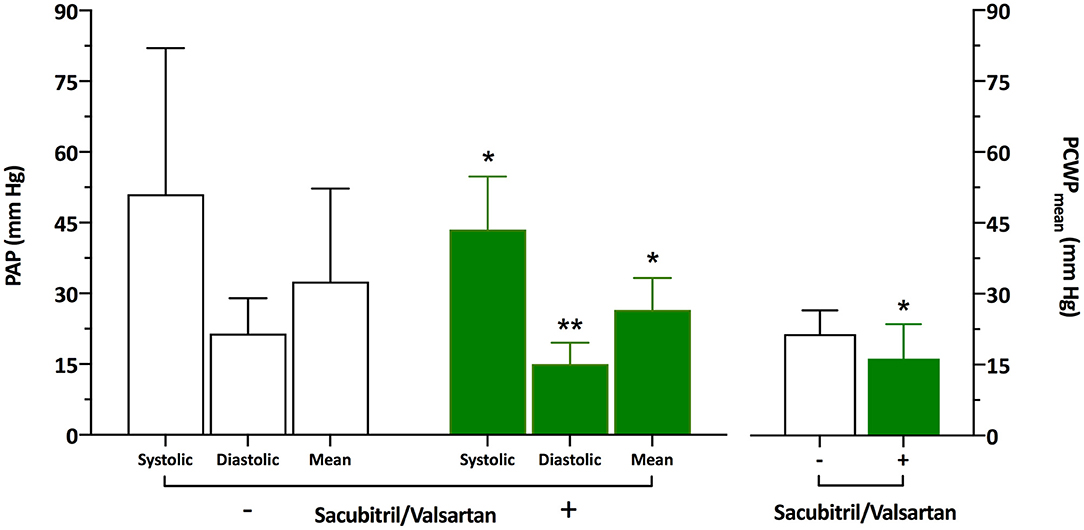
临床上,在转换为沙库巴曲/缬沙坦后,18 名患者中有 12 名的纽约心脏协会功能等级得到改善 (p<0.01)。左心室功能和心血管联合用药的超声心动图参数在使用沙库巴曲/缬沙坦之前和之后没有显着差异。
研究启示:
据文献报道,这是第一个证明沙库巴曲/缬沙坦治疗通过降低肺动脉压力改善 HFpEF 患者肺动脉高压的人体研究。尽管在进行血流动力学控制测量时患者仅接受了最低批准剂量的沙库巴曲/缬沙坦,但患者不仅在血流动力学读数方面而且在 NYHA 分类方面都经历了显着改善。沙库巴曲/缬沙坦治疗与 HFpEF 患者肺动脉高压的改善相关。
文献出处:
Burgdorf C, Brockmöller J, Strampe H, Januszewski M, Remppis BA. Reduction of Pulmonary Hypertension After Transition to Sacubitril/Valsartan in Patients With Heart Failure With Preserved Ejection Fraction. Front Cardiovasc Med. 2021 Oct 7;8:734697. doi: 10.3389/fcvm.2021.734697. PMID: 34692786; PMCID: PMC8529008.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#保留射血分数#
38
#ASC#
30
学习了!
53
#缬沙坦#
45
#Med#
38
#动脉高压#
32
认真学习了。
48
已读
48
已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读
46
谢谢分享
60