JAMA Neurol:睡眠剥夺可增加阿尔茨海默病风险
2014-06-11 佚名 丁香园
淀粉样蛋白级联假说的内容是指阿尔茨海默病(AD)最初起源于β-淀粉样(Aβ)蛋白的沉积,Aβ42蛋白是相关蛋白中最主要的成员。目前仍不清楚散发阿尔茨海默病患者中发生Aβ蛋白沉积的原因,但是这种现象被认为反映了Aβ蛋白生成和清除的失平衡。【原文下载】 流行病学调查显示了很多导致AD的潜在病因,其中有愈来愈多的证据显示睡眠不足是病因之一。机能学研究显示神经活动可增加Aβ蛋白的合成和分泌,因此清醒
淀粉样蛋白级联假说的内容是指阿尔茨海默病(AD)最初起源于β-淀粉样(Aβ)蛋白的沉积,Aβ42蛋白是相关蛋白中最主要的成员。目前仍不清楚散发阿尔茨海默病患者中发生Aβ蛋白沉积的原因,但是这种现象被认为反映了Aβ蛋白生成和清除的失平衡。【原文下载】
流行病学调查显示了很多导致AD的潜在病因,其中有愈来愈多的证据显示睡眠不足是病因之一。机能学研究显示神经活动可增加Aβ蛋白的合成和分泌,因此清醒状态(神经活动增加)可增加Aβ蛋白的生成;反之,睡眠(神经活动减少)与Aβ蛋白清除率增加和生成减少相关。
在既往研究中也确实发现,人类和啮齿动物脑脊液中Aβ蛋白水平在睡眠期比起清醒状态有着显著降低。此外,研究显示在啮齿动物中,如果清醒状态延长,可导致脑内Aβ蛋白水平增加,其沉积水平随后也同样增加。
上述研究结果提示,慢性部分睡眠剥夺导致的睡眠不足可能干扰生理性的睡眠相关脑内Aβ蛋白清除,导致持续的Aβ蛋白高浓度,并且可能导致Aβ蛋白沉积。
2014年6月2日在JAMA NEUROLOGY杂志上发表了一篇研究报告。该研究评估了健康中年男性在一晚完全睡眠剥夺(即持续清醒24小时)对脑脊液中Aβ42蛋白水平的影响。
研究者假设睡眠剥夺可导致Aβ42蛋白水平升高。因为Aβ42蛋白在Aβ蛋白空斑形成过程中起最主要作用,所以被用作本研究的主要结果参数。同时,研究者还选择了脑脊液中Aβ40蛋白、磷酸化tau蛋白(P-tau)、总tau蛋白(T-tau)作为次级结果参数;因为它们被认为是独立于Aβ蛋白起源的生物标记物,在典型AD病程晚期均会受到影响。总蛋白水平作为参照。
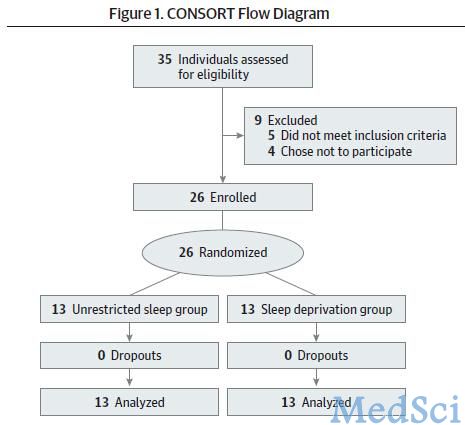
实验对象被随机分为一晚睡眠剥夺组(n=13)和自由睡眠组(n=13)。结果显示,一晚自由睡眠可清除6%的Aβ42蛋白,反之睡眠剥夺则可抵消这种清除效应。睡眠剥夺组晚间和晨间的Aβ42蛋白浓度较自由睡眠组显著升高,与此同时两组的脑脊液总蛋白水平未见明显差异。
研究显示,睡眠剥夺(或者清醒期延长)可干扰Aβ42蛋白的生理性晨间清除过程。研究者假设慢性睡眠剥夺可增加脑内Aβ42蛋白水平,从而增大患阿尔茨海默病的风险。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









学了一下,感谢
94
#Neurol#
36
#阿尔茨#
38
#阿尔茨海#
38
#阿尔茨海默#
39
#睡眠剥夺#
40