BMJ:THA术者年手术量35例可降低术后并发症
2014-06-06 伊文 丁香园
很多文献报道术者年手术量影响THA术后早期并发症(死亡、深静脉血栓、早期返修等)发生率,两者成反比关系,提示需在相对更大年手术量医院行关节置换。具体到多少例年手术量定义为低年手术量(既往文献定义少于6-52例不同),年手术量是否存在具体多少例数影响THA术后并发症,这些问题仍未解决。 加拿大Ravi医师采用限制性立方函数(restricted cubic splines)方法分析了术者年
很多文献报道术者年手术量影响THA术后早期并发症(死亡、深静脉血栓、早期返修等)发生率,两者成反比关系,提示需在相对更大年手术量医院行关节置换。具体到多少例年手术量定义为低年手术量(既往文献定义少于6-52例不同),年手术量是否存在具体多少例数影响THA术后并发症,这些问题仍未解决。
加拿大Ravi医师采用限制性立方函数(restricted cubic splines)方法分析了术者年手术量与THA术后早期90天内并发症、术后2年并发症关系,结果发表在近期的BMJ上。【原文下载】
采用国际疾病编码及加拿大疾病编码,检索加拿大4个主要患者登记数据库中2002年-2009年骨性关节炎患者首次全髋关节置换37881例(如图1),由360位主刀医师完成以上手术。

图1 排除研究标准
主要研究指标:术后早期90天并发症(深静脉血栓、肺栓塞、死亡),术后2年并发症(假体周围骨折、感染、脱位、返修);术者年手术量定义:术者在行该次置换术前一年内完成的全髋置换例数。作者统计和控制可能影响术后并发症的其他因素如年龄、性别、术前存在的内科基础疾病、社会经济地位、生活条件及环境等。
采用限制性立方函数(restricted cubic splines)方法分析每个术后并发症与术者年手术量关系(如图2),发现两者非线性关系,再通过多变量逻辑回归分析找到年手术量与并发症风险相关性分界点,发现术者年手术量35例是术后并发症风险分界点。
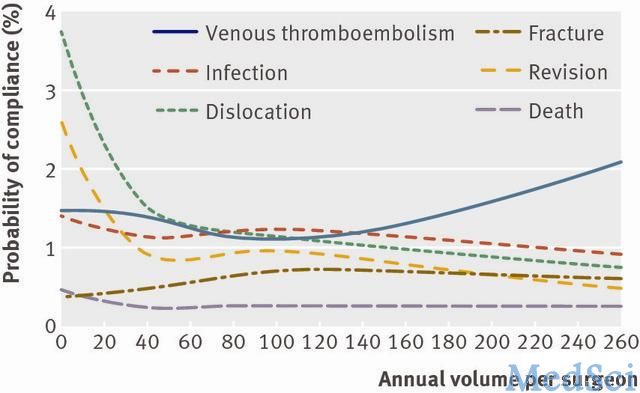
图2 年手术量与术后并发症发生率关系曲线
再以术者年手术量(≤35例或>35例)为分界点,二次匹配分析教学医院、医院年手术量、术者毕业院校、术者临床经验等影响因素。
作者发现术者年手术量与术后并发症如感染、假体周围骨折、静脉血栓、死亡方面无明显相关性;但随着年手术量增加,术后脱位及翻修风险降低。当年手术量>35例后术后脱位、翻修风险不随年手术量增加而降低,趋于稳定(如图3)。
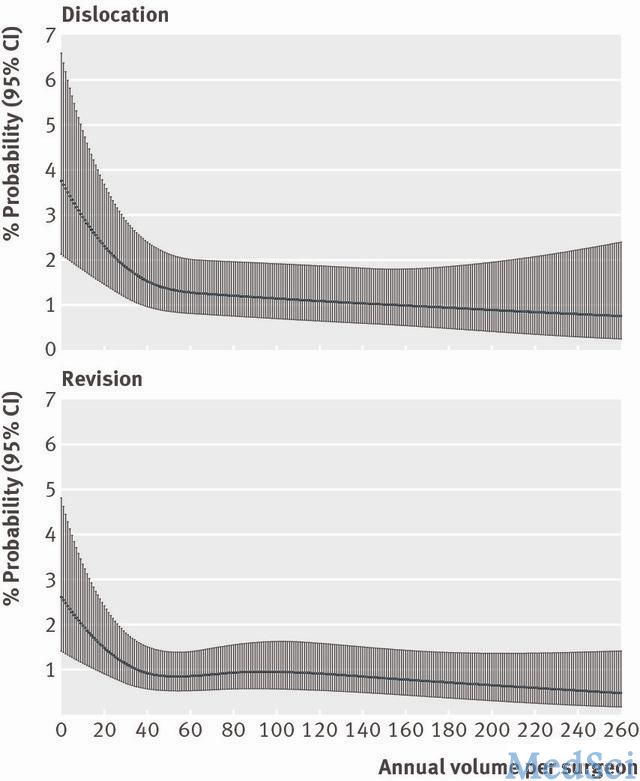
图3 上图年手术量与脱位发生率关系曲线;下图年手术量与返修发生率关系曲线
作者由此得出结论:1、患者首次全髋置换中术者年手术量≤35例,术后2年脱位、返修风险更高。本次研究未发现年手术量与术后感染、静脉血栓、假体周围骨折、死亡有明显相关性。2、术者手术量一定程度上体现了术者手术技巧,手术技巧由天赋、训练及经验造成;作者在二次分析中控制影响手术技巧的因素(毕业院校、参加临床年限)仍发现术者年手术量≤35例,术后2年脱位、返修风险更高。
外科手术术者经验与技巧很大程度决定手术成功性,全髋术后脱位、返修出现一定程度与术中假体安放位置与术中即刻稳定性相关,这些都需要术者术中决策与判断。到底多少年手术量算得“高手”,本次研究发现年手术≤35例者术后脱位、返修风险明显高于>35例者,研究样本量大,在不能排除其他影响因素时,结论仍具有可信度。
原始出处:本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#BMJ#
20
#并发#
20
#THA#
34
#手术量#
17
#手术量#
23