Cell Biosci:铜绿假单胞菌对2例COVID-19危重患者藻酸盐生物合成及VI型分泌系统的调节作用
2022-02-16 从医路漫漫 MedSci原创
新型冠状病毒肺炎对患者健康造成巨大影响,发病率和死亡率较高。
背景:新型冠状病毒肺炎对患者健康造成巨大影响,发病率和死亡率较高。在这种病毒感染基础上,肺部微生物生态的改变经常使疾病恶化,并增加宿主对重复感染的易感性。细菌重复感染加重了新冠肺炎的病情,给临床治疗带来了巨大挑战。深入研究COVID-19患者的重复感染细菌,有助于了解病毒感染后肺部微环境及重复感染机制。
中国南方科技大学第二附属医院鉴定铜绿假单胞菌为SARS-CoV-2的顶级重叠感染菌。铜绿假单胞菌是一种恶名昭著的医院感染病原体,可在囊性纤维化、呼吸机相关性肺炎(VAP)、导管相关性感染和烧伤创面等疾病的免疫低下患者中引起致命感染。重症COVID-19患者需要体外膜肺氧合(ECMO),迟发性VAP发生率非常高。铜绿脓杆菌,多次复发,难以从肺中根除病原菌。该细菌通过不同的机制引起感染,包括多种毒力因子的分泌和生物膜的形成。铜绿假单胞菌参与多种致病机制,包括群体感应系统、蛋白分泌系统、胞外多糖等,在多种微生物环境中竞争并逃脱宿主的免疫攻击。聚敛演化的纵向分析。慢性肺部感染的临床分离铜绿假单胞菌表明,生物膜形成和毒力因子的重塑是宿主适应的必要条件。mucA、vgrG、lasR、rpoN和pvdS等基因的突变会显著损害群体感应系统、蛋白分泌系统和毒力因子的生物合成,并在囊性纤维化和呼吸机相关性肺炎等肺部疾病患者中,铜绿假单胞菌逃避宿主免疫清除。在蛋白质分泌系统中,VI型分泌系统(T6SS)对铜绿假单胞菌与其他微生物竞争,损害宿主细胞。对这些进化特征的分析可能有助于治疗绿脓杆菌。
结果:分析了两种绿脓杆菌。结合测序分析和表型分析,从2例COVID-19危重患者中分离出具有相同MLST型的铜绿假单胞菌菌株。研究发现,铜绿假单胞菌在COVID-19患者短期定植期间启动海藻酸盐生物合成并减弱VI型分泌系统(T6SS),导致生物膜过度形成和毒力降低—慢性感染的两个不同标记物。巨噬细胞毒性试验和细胞内活性氧测定证实了绿脓杆菌的存在。铜绿假单胞菌菌株降低了它们对宿主细胞的毒力,比它们的祖先更好地逃避宿主的免疫清除。
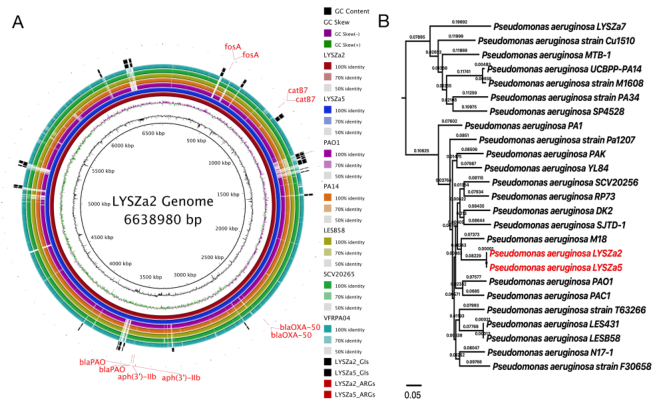
图1 LYSZa2和LYSZa5的环部图及系统进化树。LYSZa2和LYSZa5与其他P。绿脓杆菌基因组。从最里面开始,环1:GC内容(黑色);环2:GC歪斜(紫色/绿色);环3:LYSZa2(暗红色);环4:LYSZa5(海军);环5:PAO1实验室参比菌株(紫色);环6:PA14临床强毒株(橙色);环7:来自CF患者的LESB58高毒临床菌株(橄榄色);环8:SCV20265小菌落变异株(浅绿色);环9:来自角膜炎患者的VRFPA04多药耐药株(青色);环10和11:LYSZa2和LYSZa5上的GIs(黑色);环12和13:LYSZa2和LYSZa5上的ARGs(红色);B基于核心基因组比对,利用LYSZa2和LYSZa5基因组与其他23个P. aeruginosa基因组构建系统发育树,LYSZa2和LYSZa5用红色高亮显示
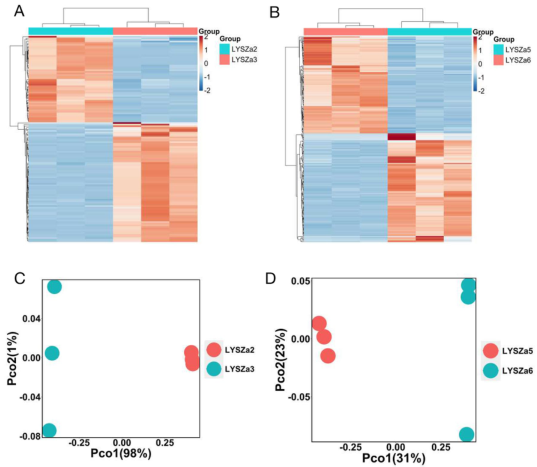
图2遗传分离株与子代分离株间DEGs的热图和PCoA图。LYSZa3与LYSZa2中显著DEGs的Heatmap图;与LYSZa5相比,LYSZa6中显著DEGs的B热图;利用Bray Curtis dissimilarity法绘制LYSZa3组和LYSZa2组基于DEGs的C PCoA图;利用Bray Curtis dissimilarity法,根据DEGs绘制LYSZa6组和LYSZa5组的D PCoA图
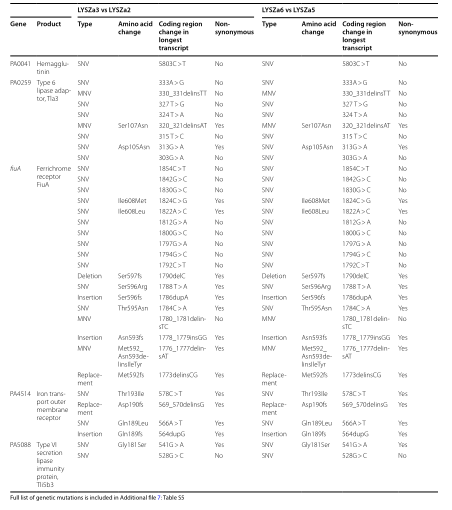
表1 LYSZa3和LYSZa6之间常见的基因突变
结论:我们的研究表明,SARS-CoV-2感染可以创造一个更适合生存的肺部环境,允许具有适合慢性感染的遗传特征的细菌病原体快速适应并且进化。
原文出处: Qu J, Cai Z, Duan X,et al.Pseudomonas aeruginosa modulates alginate biosynthesis and type VI secretion system in two critically ill COVID-19 patients.Cell Biosci 2022 Feb 09;12(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
53
#分泌#
42
#Cell#
36
#Bio#
48
好
52
学习啦
60