Nature提出细胞自毁新学说
2015-06-25 何嫱 生物通
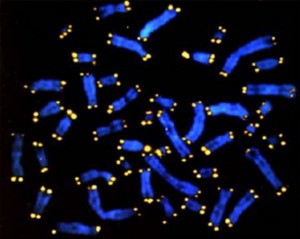
我们染色体末端的特殊结构——端粒决定了细胞可以在多长的时间里继续复制自身。长期以来人们一直在研究它与衰老过程和癌症的关联。现在来自Salk研究所的一个研究发现表明,在细胞阻止肿瘤的自毁程序中端粒有可能比以往认为的要更加重要,有可能可以利用这一功能来改善癌症治疗。这项研究发布在《自然》(Nature)杂志上。当细胞在有丝分裂过程中进行复制时,它们的端粒每次都会缩短一点点。最终,在多次的细胞分裂后,端
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
28
这篇文章有一定深度
109
是一篇不错的文章
117
真是好网站
93
新视角,新方向!
118
厉害
132
肿瘤完蛋了
70
厉害
125
牛气
74
新学说可能是质的飞跃
75