JACC:二尖瓣反流:经皮修复和手术效果相当(5年随访结果)
2015-12-22 cuiqian译 MedSci原创
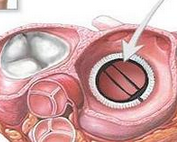
在EVEREST II(血管内瓣膜边缘对边缘修复研究)研究中,用一个新的经皮装置治疗二尖瓣反流(MR)安全性优于外科手术,但在1年时MR减少不太有效。本研究旨在评估与传统的MV手术相比,MitraClip设备最后5年的临床结果和经皮二尖瓣(MV)修复的耐用性。3+或4+级的MR患者被随机接受用该设备进行经皮修复或常规的MV手术,以2:1的比例进行分配(178:80)。患者前瞻性同意进行5年的随访。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#5年随访#
37
#JACC#
38
#随访结果#
38
难道心外就是走射线这条路了
129
是一篇不错的文章
134
这篇文章有一定深度
130
已经收藏…
87
感谢分享,
103
好文章,
163
值得分享,
101