经典永流传-Pit Pattern分类,测一测你能否正确诊断?
2020-04-15 com0707 一泓小树林
经典永流传-Pit Pattern分类,测一测你能否正确诊断?

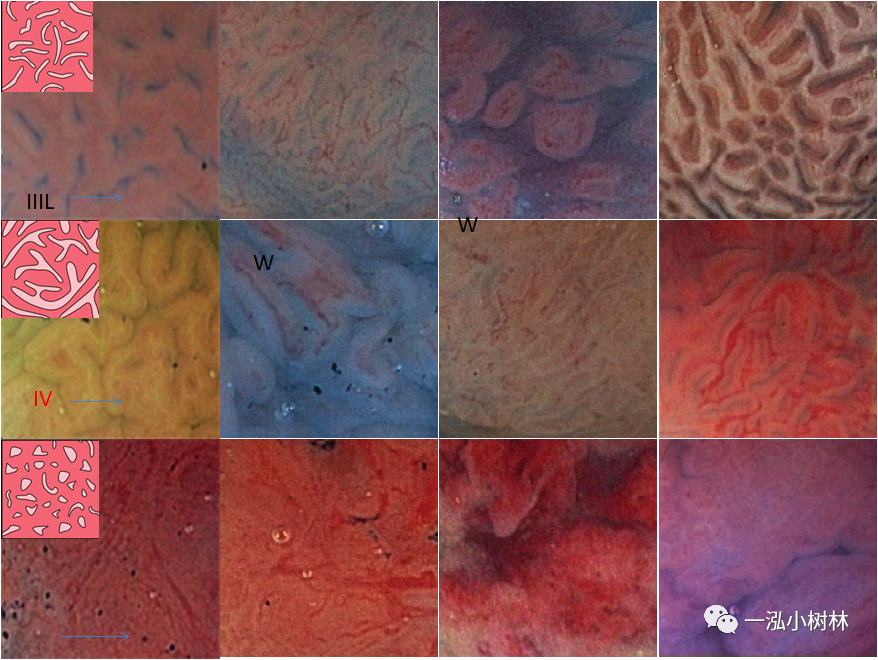
图1 Pit Pattern 放大色素内镜分类

图2 Pit Pattern 色素内镜分类
Pit Pattern I型
 图3 结肠正常黏膜放大图像,可见圆形小pit,为正常隐窝。
图3 结肠正常黏膜放大图像,可见圆形小pit,为正常隐窝。
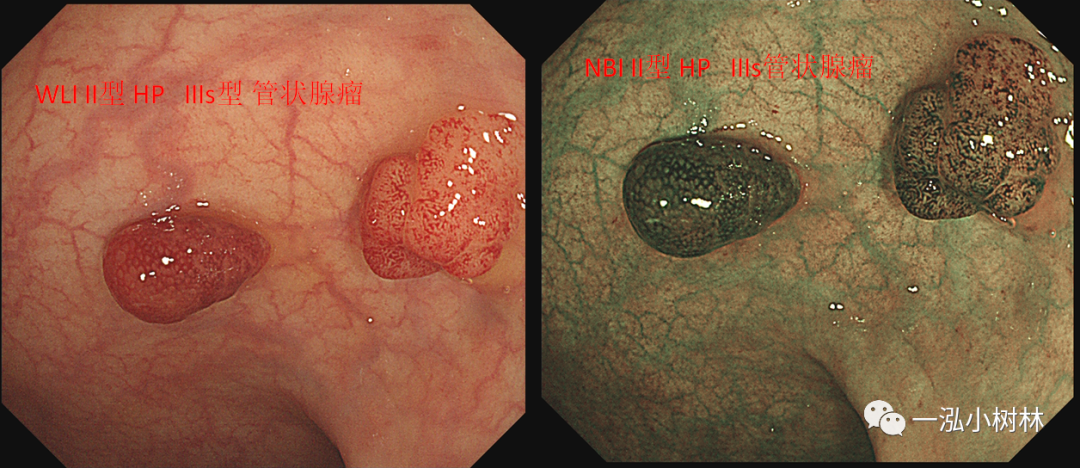
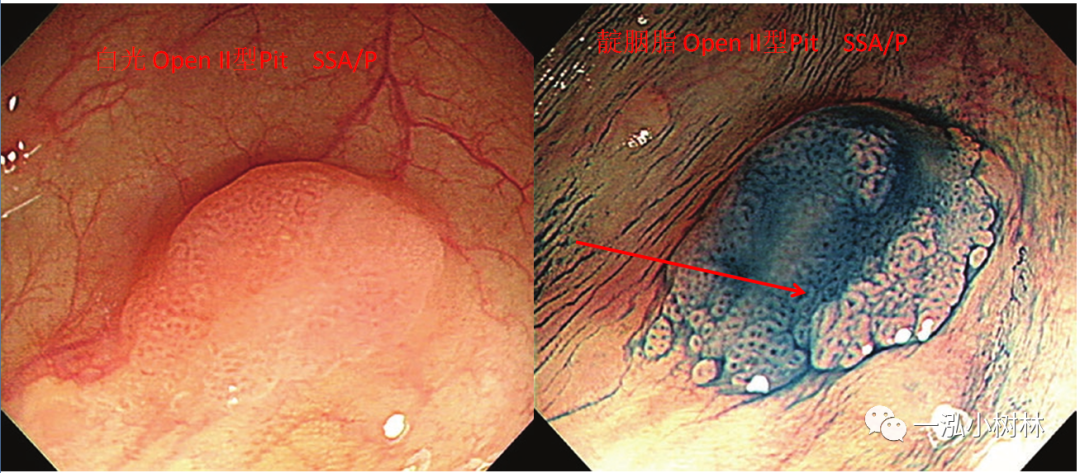
Pit Pattern II型
 图4 典型的 pit pattern II型,具有星形或洋葱皮状结构(左),II型开放 pit pattern由于黏液生成导致隐窝打开是SSA/P的特征(右)。
图4 典型的 pit pattern II型,具有星形或洋葱皮状结构(左),II型开放 pit pattern由于黏液生成导致隐窝打开是SSA/P的特征(右)。
Pit Pattern IIIs型
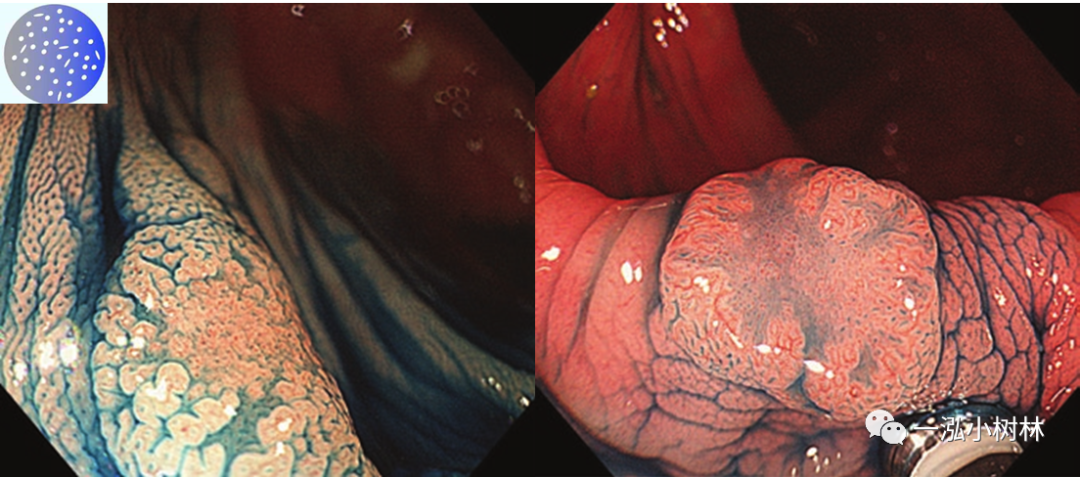 图5 pit pattern III型由小的管状或圆形pits组成,比正常黏膜周围的隐窝小。
图5 pit pattern III型由小的管状或圆形pits组成,比正常黏膜周围的隐窝小。
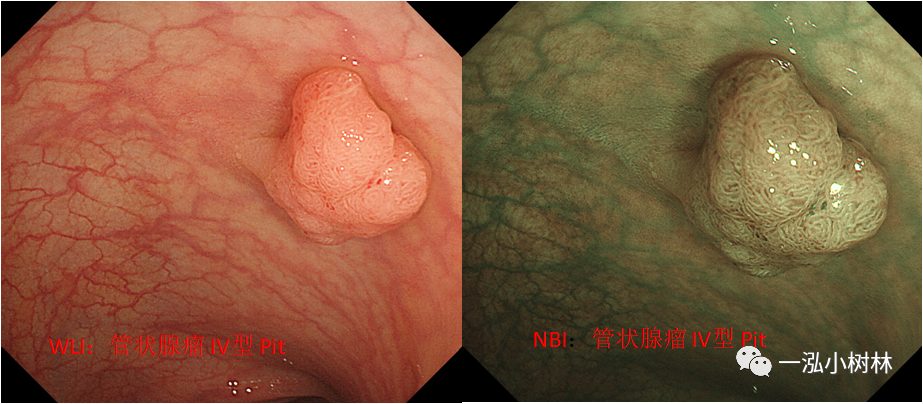
Pit Pattern IIIL型
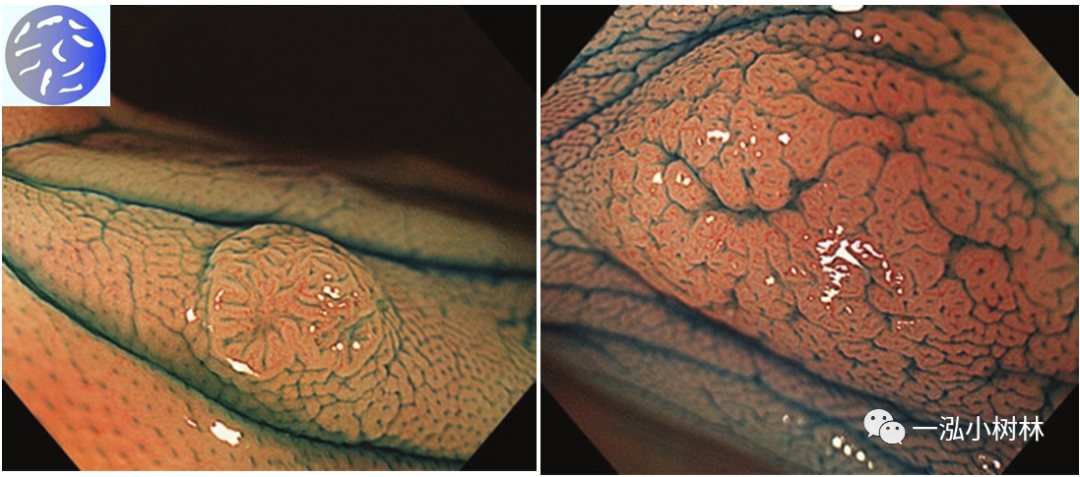 图5 pit pattern IIIL型由长管状隐窝组成(左),有时在内部区域与正常隐窝混合在一起(右)。
图5 pit pattern IIIL型由长管状隐窝组成(左),有时在内部区域与正常隐窝混合在一起(右)。
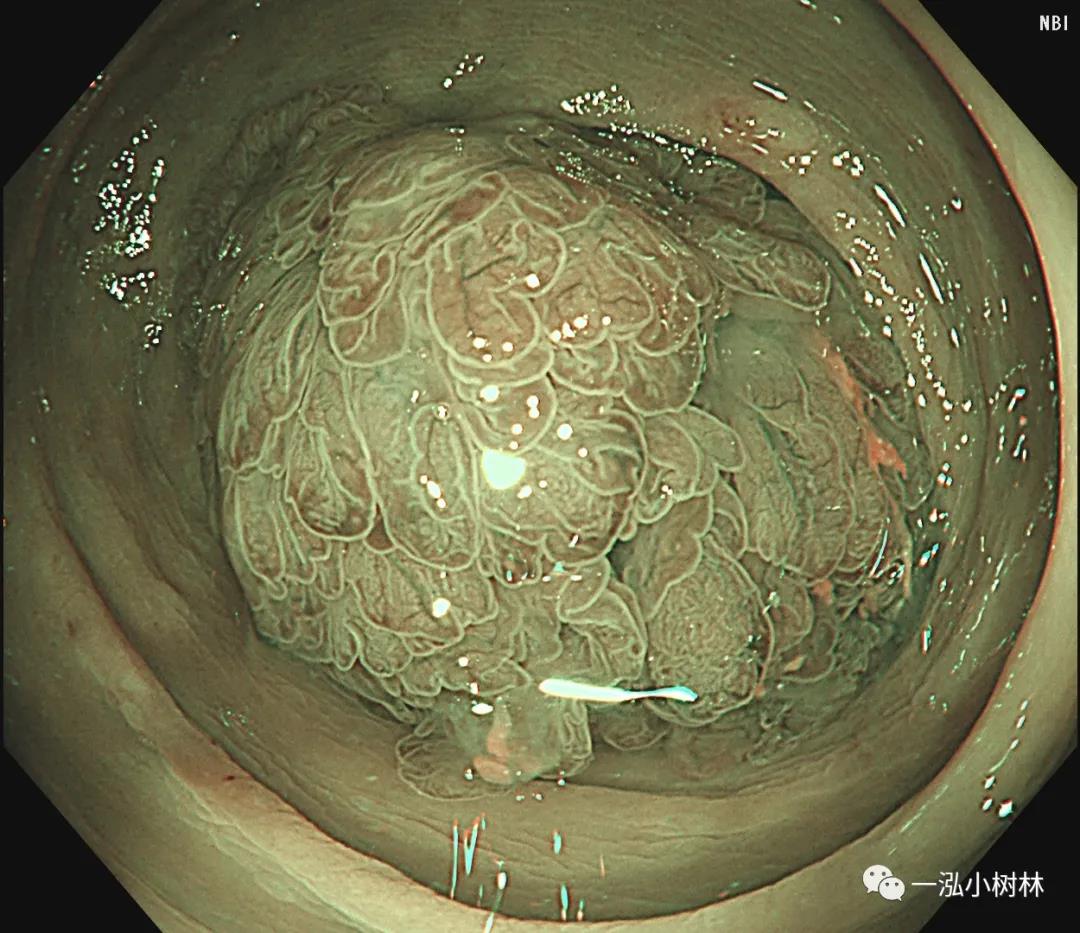
Pit Pattern IV型
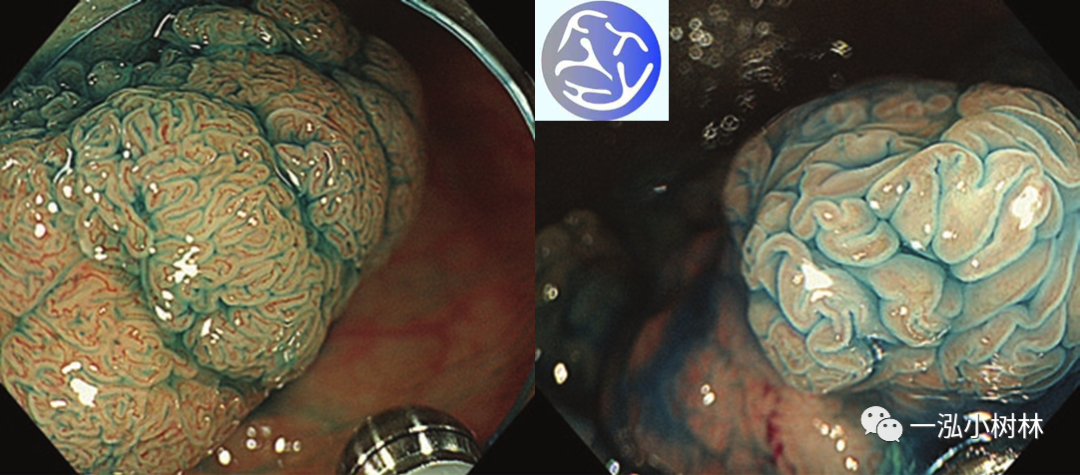 图6 pit pattern IV型为沟状、分支状或脑回样的表面结构。
图6 pit pattern IV型为沟状、分支状或脑回样的表面结构。
Pit Pattern VI型
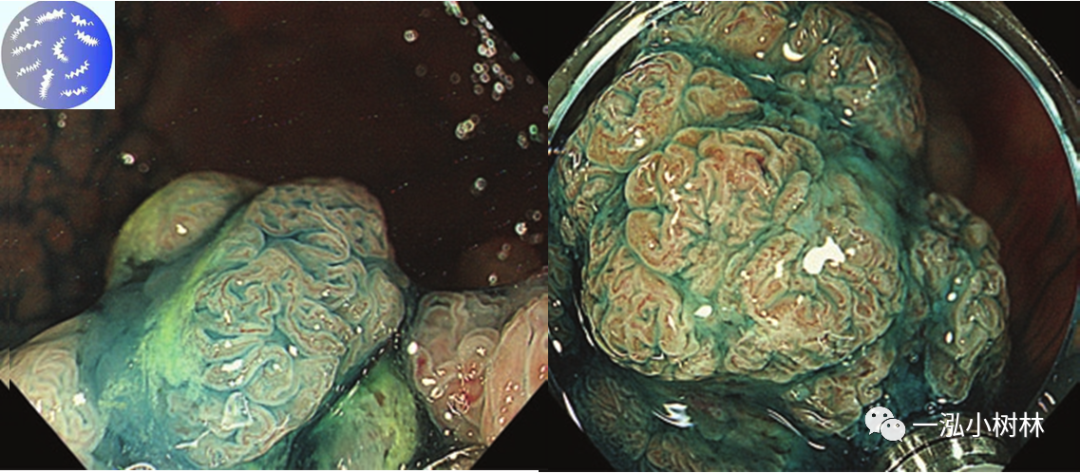 图7 pit pattern VI型与IIIL、IIIS和IV型类似,但由无序性、大小不等、不对称的腺管等组成。轻度不规则的称为“低级”(左),高度不规则的为“高级”(右)。
图7 pit pattern VI型与IIIL、IIIS和IV型类似,但由无序性、大小不等、不对称的腺管等组成。轻度不规则的称为“低级”(左),高度不规则的为“高级”(右)。
Pit Pattern VN型
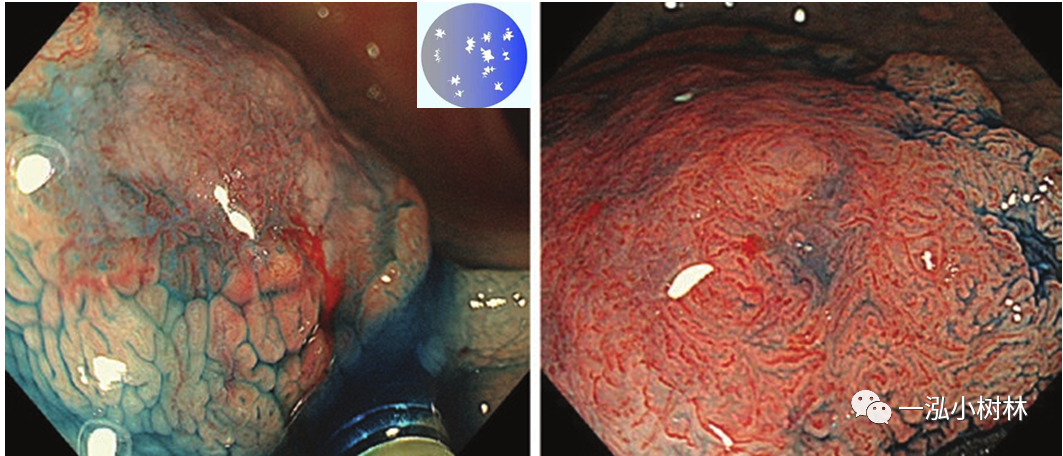 图8 pit pattern VN型指表面结构丢失(左侧)或破坏(右侧) 。
图8 pit pattern VN型指表面结构丢失(左侧)或破坏(右侧) 。
Pit Pattern分类的意义
内镜诊断是内镜最重要的组成部分。使用放大内镜用于“Pit诊断”,更接近病理诊断。在Pit Pattern分类中,肿瘤与非肿瘤之间的正确诊断率约为96%~98%,腺瘤与癌症之间的正确识别率约为70%~90%。在黏膜下浸润癌中,血管浸润和淋巴结转移的风险与肿瘤的垂直浸润(T1)成正比。因此,在内镜下治疗早期结直肠癌之前,有必要对其浸润深度进行诊断。放大内镜显示,当作为Vn型黏膜下层侵犯的指标时,正确的识别率约为90%。因此,用放大内镜可以获得高精度的定性诊断。
 白光+NBI
白光+NBI
白光+NBI
白光+靛胭脂

白光内镜 CF-HQ290I
NBI CF-HQ290I
靛胭脂 CF-HQ290I
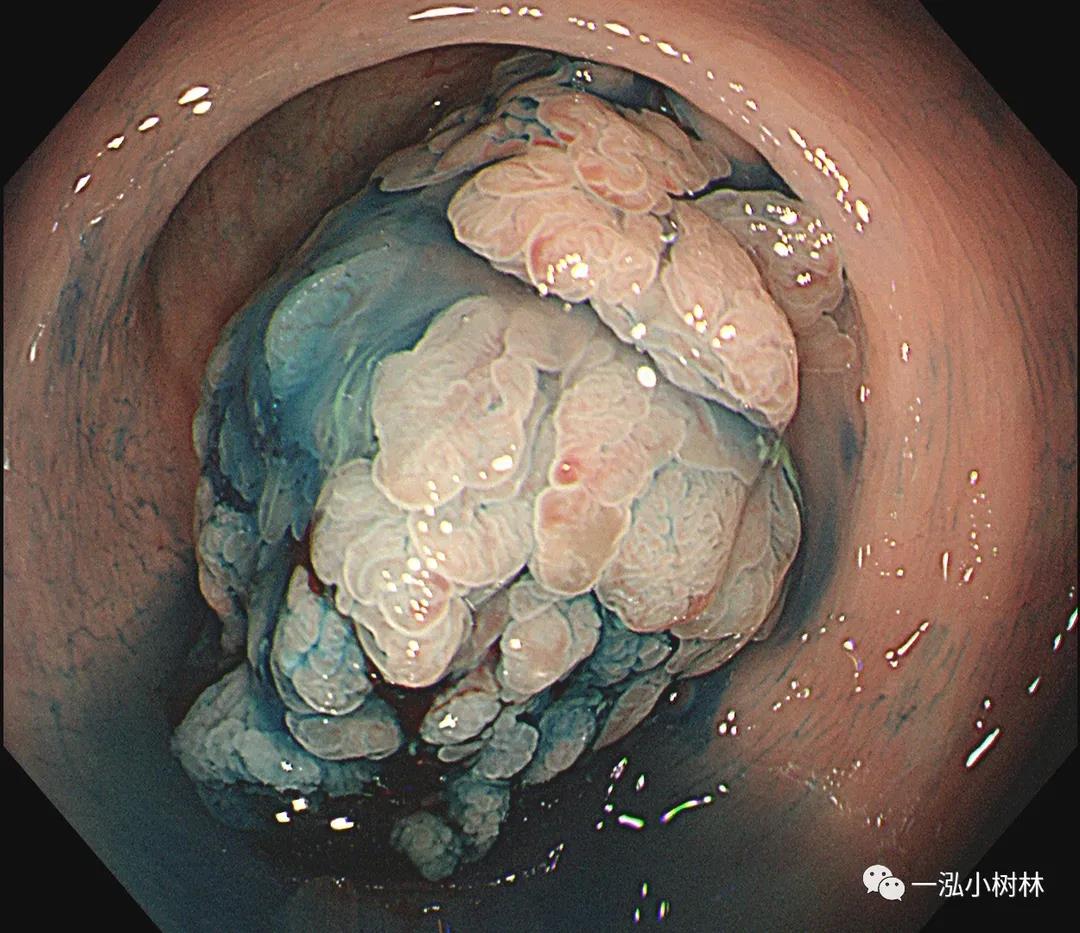
以下几张图片你的诊断是腺管分型?绒毛管状腺瘤或者TSA?
 白光内镜 CF-H260I
白光内镜 CF-H260I
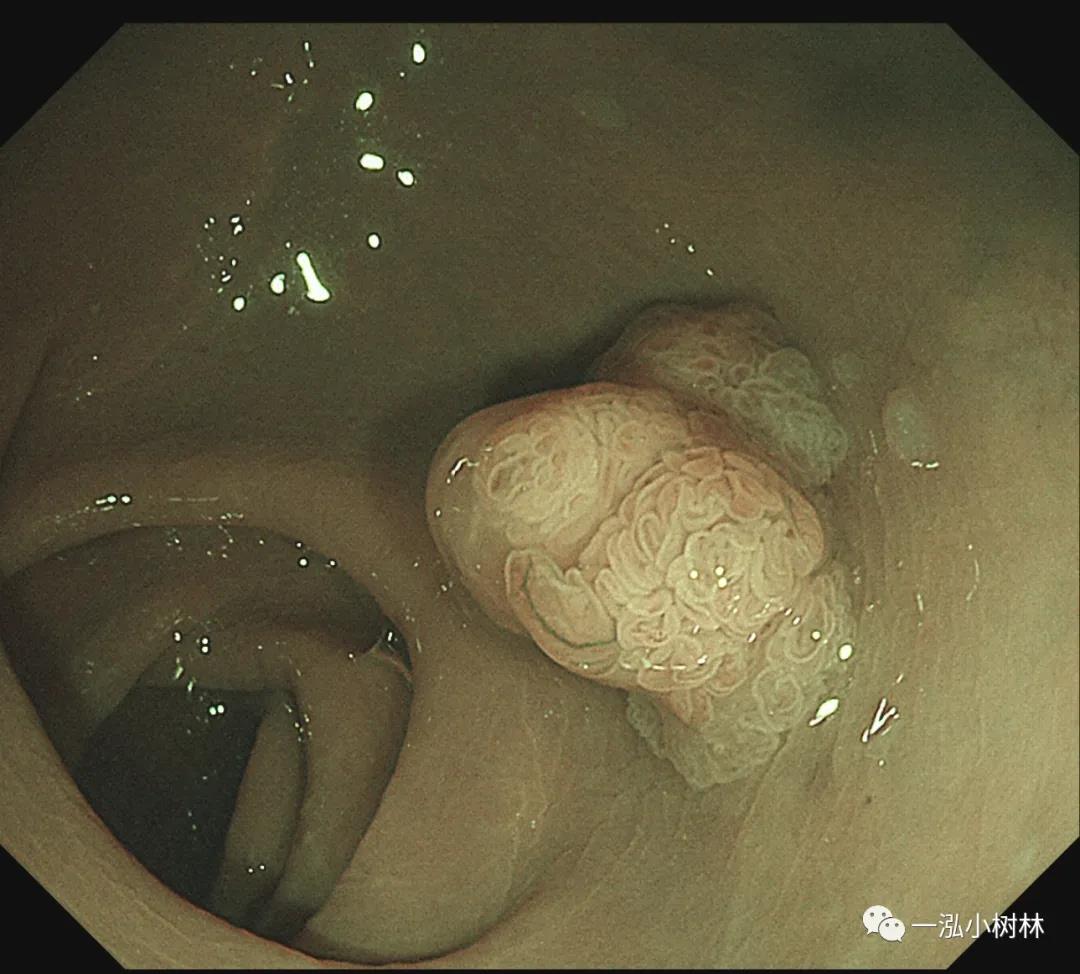
NBI CF-H260I

靛胭脂 CF-H260I

NBI CF-H260I

甲紫染色 CF-H260I
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#pattern#
60
高压
100
#Pit Pattern分类#
40
#TTE#
61