NEJM:扁桃体切除术可治疗儿童OSAS
2013-06-21 青楚 医学论坛网
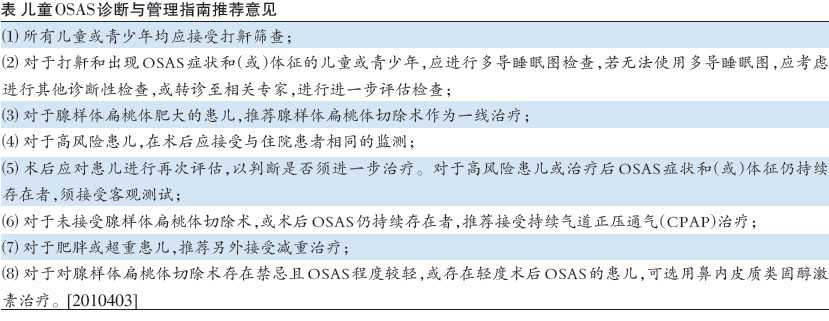
扁桃体切除术通常用于治疗阻塞性睡眠呼吸暂停综合征(OSAS)儿童,但对于减轻症状、改善认知、行为和生活质量并无效果,多导睡眠图结果也尚未被严格评估。美国学者假设在没有持续血样饱和度下降、早期扁桃体切除的OSAS儿童中,比较观察等待和积极治疗的效果。相关论文2013年6月20日在线发表于《新英格兰医学杂志》(N Engl J Med)。 该研究随机分配464例
扁桃体切除术通常用于治疗阻塞性睡眠呼吸暂停综合征(OSAS)儿童,但对于减轻症状、改善认知、行为和生活质量并无效果,多导睡眠图结果也尚未被严格评估。美国学者假设在没有持续血样饱和度下降、早期扁桃体切除的OSAS儿童中,比较观察等待和积极治疗的效果。相关论文2013年6月20日在线发表于《新英格兰医学杂志》(N Engl J Med)。
该研究随机分配464例5-9岁的OSAS患儿,安排早期扁桃体切除术或观察等待。研究开始和7个月的时候分别测量多导睡眠图、认知、行为和健康状况。
结果显示,早期扁桃体切除术 可以改善儿童OSAS患者的多项指标,但缺乏循证医学证据。与病情观察随访的患儿相比,手术治疗在改善注意力或执行能力上无明显优势,但手术的确有助于改善症状、生活质量和多导睡眠图等,因此研究者仍推荐早期手术。

A Randomized Trial of Adenotonsillectomy for Childhood Sleep Apnea
Background
Adenotonsillectomy is commonly performed in children with the obstructive sleep apnea syndrome, yet its usefulness in reducing symptoms and improving cognition, behavior, quality of life, and polysomnographic findings has not been rigorously evaluated. We hypothesized that, in children with the obstructive sleep apnea syndrome without prolonged oxyhemoglobin desaturation, early adenotonsillectomy, as compared with watchful waiting with supportive care, would result in improved outcomes.
Methods
We randomly assigned 464 children, 5 to 9 years of age, with the obstructive sleep apnea syndrome to early adenotonsillectomy or a strategy of watchful waiting. Polysomnographic, cognitive, behavioral, and health outcomes were assessed at baseline and at 7 months.
Results
The average baseline value for the primary outcome, the attention and executive-function score on the Developmental Neuropsychological Assessment (with scores ranging from 50 to 150 and higher scores indicating better functioning), was close to the population mean of 100, and the change from baseline to follow-up did not differ significantly according to study group (mean [±SD] improvement, 7.1±13.9 in the early-adenotonsillectomy group and 5.1±13.4 in the watchful-waiting group; P=0.16). In contrast, there were significantly greater improvements in behavioral, quality-of-life, and polysomnographic findings and significantly greater reduction in symptoms in the early-adenotonsillectomy group than in the watchful-waiting group. Normalization of polysomnographic findings was observed in a larger proportion of children in the early-adenotonsillectomy group than in the watchful-waiting group (79% vs. 46%).
Conclusions
As compared with a strategy of watchful waiting, surgical treatment for the obstructive sleep apnea syndrome in school-age children did not significantly improve attention or executive function as measured by neuropsychological testing but did reduce symptoms and improve secondary outcomes of behavior, quality of life, and polysomnographic findings, thus providing evidence of beneficial effects of early adenotonsillectomy. (Funded by the National Institutes of Health; CHAT ClinicalTrials.gov number, NCT00560859.)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#扁桃体切除#
34
#扁桃体切除术#
44
#OSAS#
43
#SAS#
39
#切除术#
32
#OSA#
20