Eur Heart J:脂蛋白(a)与主动脉瓣钙化相关
2022-07-25 MedSci原创 MedSci原创
Lp(a)浓度与基线和新发AVC密切相关,但与AVC进展无关,这表明降低Lp(a)的措施可能在主动脉瓣疾病钙化前阶段最为有效。
脂蛋白(a)[Lp(a)]是主动脉瓣疾病发病的潜在致病因素。然而,Lp(a)与新发主动脉瓣钙化(AVC)、AVC进展的关系尚未明确。

近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,该研究旨在评估高血清Lp(a)水平是否与AVC的发生和进展相关。

基于人群的鹿特丹研究共有922名参与者(平均年龄为66.0±4.2岁,47.7%为男性),他们的Lp(A)检查结果可用,基线时接受了非增强心脏计算机断层成像检查。中位随访时间为14.0[四分位差(IQR)为13.9-14.2]年。新发AVC定义为:第一次扫描无AVC时,后续随访扫描AVC评分>0。AVC评分在基线和随访扫描之间的绝对差值被定义为进展。研究人员采用Logistic和线性回归分析评估Lp(a)水平与基线AVC、新发AVC和进展的关系。所有分析都调整了年龄、性别、体重指数、吸烟、高血压、血脂异常和肌酐水平。

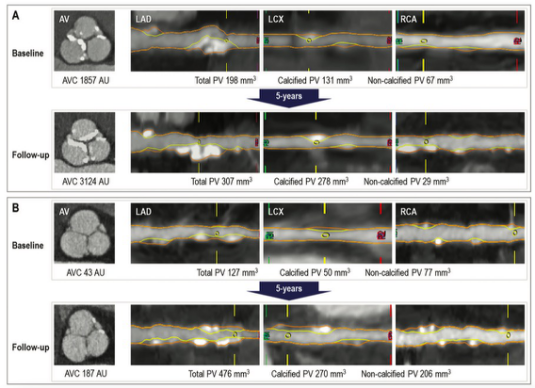
在702名基线无AVC的参与者中,415名(59.1%)参与者在后续随访扫描中出现新发AVC。在基线AVC参与者中,年度进展中位数为13.5(IQR=5.2-37.8)Agatston单位(AU)。Lp(a)浓度与基线AVC[Lp(a)每升高50mg/dL的比值比(OR)为1.43;95%可信区间(CI)为1.15-1.79]和新发AVC(Lp(a)每升高50mg/dL,OR为1.30;95%CI为1.02-1.65)独立相关,但不伴有AVC进展(β:−71AU,Lp(a)每增加50mg/dL;95%CI为−117;35)。只有基线AVC评分与AVC进展显著相关(P<0.001)。
由此可见,在以人群为基础的鹿特丹研究中,Lp(a)浓度与基线和新发AVC密切相关,但与AVC进展无关,这表明降低Lp(a)的措施可能在主动脉瓣疾病钙化前阶段最为有效。
原始出处:
Yannick Kaiser,et al.Lipoprotein(a) is associated with the onset but not the progression of aortic valve calcification Get access Arrow.European Heart Journal.2022.https://academic.oup.com/eurheartj/advance-article-abstract/doi/10.1093/eurheartj/ehac377/6649081?redirectedFrom=fulltext
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#主动脉瓣#
53
#ART#
34
#主动脉#
46
#脂蛋白#
64
#HEART#
39
#主动脉瓣钙化#
43