解读:2016 WHO中枢神经系统肿瘤分类
2017-01-17 复旦大学附属华山医院放射科 中华放射学杂志
作者:复旦大学附属华山医院放射科(任彦、吴越、庞浩鹏、狄宁宁、解骞、张家文、张俊海、刘含秋、冯晓源、姚振威),病理科(汪寅);山东大学齐鲁医院放射科(李安宁) WHO于2016年5月9日在Acta Neuropathol 杂志发表了中枢神经系统肿瘤的新分类方法(简称2016 CNS WHO肿瘤分类)。笔者将从影像医学的角度来解读此新分类方法对中枢神经系统肿瘤的诊断和治疗产生的影响。2
作者:复旦大学附属华山医院放射科(任彦、吴越、庞浩鹏、狄宁宁、解骞、张家文、张俊海、刘含秋、冯晓源、姚振威),病理科(汪寅);山东大学齐鲁医院放射科(李安宁)
WHO于2016年5月9日在Acta Neuropathol 杂志发表了中枢神经系统肿瘤的新分类方法(简称2016 CNS WHO肿瘤分类)。笔者将从影像医学的角度来解读此新分类方法对中枢神经系统肿瘤的诊断和治疗产生的影响。2016 CNS WHO肿瘤分类相对于2007版分类是概念和实践上的双重改进。
新分类首次在常规组织学特征基础上增加分子分型来对CNS肿瘤进行定义,从而提出了在分子病理时代对CNS肿瘤进行分类、诊断的新概念。影像医学和病理学都是以组织形态为本的诊断技术。
在过去的一个世纪,脑肿瘤的病理分类主要基于肿瘤的组织学特征,例如,2007 版CNSWHO肿瘤分类中仅将星形细胞表型同少突胶质细胞表型进行了组织学区分。在过去的20年里,随着肿瘤发生的共同遗传学基础以及一些少见脑肿瘤的特殊遗传学基础被逐步阐明,对脑肿瘤进行分子亚型归类成为可能。
2014年,在荷兰哈勒姆举办的国际神经病理协会会议上,神经病理学家们讨论并制订了如何将分子信息整合进入脑肿瘤诊断的指南,从而奠定了对2007版CNS WHO肿瘤分类进行修改的基础。2016 CNS WHO肿瘤分类打破了仅依靠显微镜对脑肿瘤进行病理分类的原则,将分子信息整合进入脑肿瘤诊断,并据此对CNS肿瘤分类进行了更新。今天病理学已经达到分子和基因水平,迈入了精准医学的大门。
在过去30多年的发展中,影像医学在传统的组织病理学诊断中发挥了重要的作用,胶质瘤影像学与组织病理学的诊断几乎一致。然而,随着神经肿瘤分子病理诊断时代的到来和分子生物学的突破进展,影像医学是否还能跟上分子病理学的步伐,在无创整合诊断中继续发挥作用,是精准医学背景下现代影像医学亟待解决的新课题。2016 CNS WHO 肿瘤分类官方定义其为2007版(第4版)的修订版而不是第5版,所以第5版的WHO蓝皮书并没有出版。
一、2016 CNS WHO肿瘤分类的主要变化
2016 CNS WHO肿瘤分类较2007版有大量的更新,最主要的变化包括:(1)确立在分子病理时代诊断CNS肿瘤的新概念;(2)弥漫型胶质瘤大范围重新分类,整合入基因诊断的新病种;(3)髓母细胞瘤大范围重新分类,整合入基因诊断的新病种;(4)其他胚胎性肿瘤大范围重新分类,整合入基因诊断的新病种,并去除了“原始神经外胚层肿瘤”的术语。
新的分类方法最鲜明的特点是对部分肿瘤如星形细胞瘤和髓母细胞瘤提出了分层诊断的概念,包括:层次1,组织分类(histology classification);层次2,WHO 分级(WHO grade);层次3,分子信息(molecular information);层次4,整合诊断(integrated diagnosis)。为适应这个转变,影像医学不仅需要对原先的CNS肿瘤影像特征进行重新整理,更需要紧密结合病理进行深入的功能和基因影像学研究。
2016 CNS WHO 肿瘤分类整合组织学特征和分子基因型信息的方法增加了CNS肿瘤诊断的客观性,能更精确地提示患者预后和改善疗效,但同时也产生了不能被归为其中任何一种诊断的分类。一个典型的例子就是有关少突星形细胞瘤的诊断。新的分类诊断由于联合了分子基因型和组织表型,使这类肿瘤的大部分都可以根据IDH-突变(包括IDH1和IDH2)、ATRX缺失、TP53阳性和1p/19q 共缺失的状态被诊断为弥漫星形细胞瘤(IDH突变、ATRX缺失、TP53阳性)或少突胶质细胞瘤(IDH突变、1p/19q共缺失),但也产生了部分在同一肿瘤内部兼具少突胶质细胞瘤和弥漫星形细胞瘤组织特征和基因表型的“纯正”少突星形细胞瘤诊断。
2016 CNS WHO 肿瘤分级标准依旧以组织学为基础。但是随着对基因信息的深入了解,将来弥漫型胶质瘤的WHO分型对组织学信息的依赖可能会逐渐降低。目前,联合了组织表型和基因型的2016 CNS WHO 肿瘤分类正全面进入“整合”诊断时代。但在一些无法进行分子诊断检测的医学中心,一些肿瘤类型可归为无特殊指定(not otherwisespecified,NOS),主要指没有足够的信息分类到更特定病种的肿瘤。该分类不仅包括了没有进行相关基因检测的肿瘤,还包括一小部分虽然进行了基因检测,但是没有发现与诊断相关的基因型改变的肿瘤。
2016 CNS WHO肿瘤分类对弥漫型胶质瘤、髓母细胞瘤及其他胚胎性肿瘤进行了大范围重新分类,而如何利用影像医学对这些新分类进行归纳总结,继续发挥影像医学的无创诊断价值,指导临床治疗和改善CNS肿瘤患者预后,值得广大影像医学工作者们进一步的深入思考和探讨。最近的文献报道提示影像医学已经在CNS肿瘤整合诊断的道路上进行了诸多有益的探索,包括弥漫型胶质瘤、髓母细胞瘤以及其他CNS肿瘤。
二、2016 CNS WHO肿瘤分类与影像医学
1. 弥漫型胶质瘤:对弥漫型胶质瘤,新分类最显著的变化是将所有弥漫浸润型胶质瘤(无论是星形细胞还是少突胶质细胞)归于一类,不同于过去将所有星形细胞瘤归于一类。新分类方法在传统组织学表型的基础上,整合入肿瘤的分子基因型,如IDH基因的突变状态。新分类中弥漫型胶质瘤包括星形细胞瘤(WHO Ⅱ级和Ⅲ级)、少突胶质细胞瘤(WHO Ⅱ级和Ⅲ级)、胶质母细胞瘤(WHO Ⅳ级)以及儿童相关的弥漫型胶质瘤。
如何在整合了分子基因型的弥漫型胶质瘤分类和分级诊断中继续发挥作用,并找到合适的影像学标记物对IDH基因突变亚型做出预测,是影像医学发展目前亟待解决的问题。MR研究提示IDH基因突变型胶质瘤较野生型具有一定的特征性,如胶质瘤氢质子MRS研究显示IDH突变的下游代谢产物2-羟基戊二酸(2-hydroxyglutarate,2-HG)在2.25ppm位置有特异性的波峰出现(图1~3),而且通过定量分析显示IDH2突变相比IDH1突变产生了更多的2-HG。另外,弥漫型胶质瘤MR灌注加权成像研究也表明较低的相对脑血容量(relativecerebral blood volume, rCBV)是IDH 突变型弥漫型胶质瘤(WHO Ⅱ、Ⅲ级)区别于野生型的重要功能影像特征,利用rCBV可以对弥漫型胶质瘤(WHOⅡ、Ⅲ级)的IDH突变亚型做出预测。

图1~3 男,36岁,右颞叶少突胶质细胞瘤Ⅱ级,IDH-突变,1p19q-完整。多体素MRS横断面液体衰减反转恢复(FLAIR)T2WI定位相(图1)提示47(图2)和48(图3)两个ROI在横坐标2.25 ppm(×10-6)处均可见高耸的2-羟基戊二酸(2-HG)
2. 弥漫型星形细胞瘤和间变型星形细胞瘤:WHO Ⅱ级弥漫型星形细胞瘤和WHO Ⅲ级间变型星形细胞瘤在新分类中都各自分为IDH突变型、IDH野生型和NOS 3类。传统上,WHO Ⅱ级弥漫型星形细胞瘤和WHO Ⅲ级间变型星形细胞瘤预后差别是非常显著的。但是,最近的一些研究提出IDH突变的WHOⅡ级弥漫型星形细胞瘤和IDH突变的WHO Ⅲ级间变型星形细胞瘤的预后差别并非很显著。
目前,对于IDH突变型和野生型的星形细胞瘤仍然推荐保留WHO分级。尽管大脑胶质瘤病作为一个独立的诊断病种已从2016 CNS WHO 肿瘤分类中删除,但其作为一种生长模式,却存在于多种胶质瘤中,包括IDH突变型星形细胞瘤和少突胶质细胞瘤以及IDH野生型胶质母细胞瘤。根据MR检查中肿瘤是否强化以及扩散受限程度可以对WHO Ⅱ级和Ⅲ级弥漫型星形细胞瘤进行准确分级。有研究显示MR灌注加权成像的rCBV 值预测IDH 突变型胶质瘤的准确性为88%(WHO Ⅱ、Ⅲ级),其主要原理为IDH突变代谢物2-HG 与保持低氧诱导因子(hypoxia-inducingfactor-1A,HIF-1A)的低水平有关;而HIF-1A 是肿瘤血管生成的重要诱导因子,因此,IDH突变的胶质瘤可能具有比野生型相对较低的rCBV水平。更近的一项研究提示,扩散加权成像技术(如DTI和DWI)可以鉴别不同级别弥漫型星形细胞瘤的IDH1(R132H)突变状态。
这些研究都为术前利用影像学方法进行胶质瘤的非侵入性整合诊断提供了临床应用的可能性。
3. 胶质母细胞瘤:2016 CNS WHO肿瘤分类将胶质母细胞瘤分为3种类型:(1)胶质母细胞瘤,IDH-野生型(约占90%),与临床所定义的原发性胶质母细胞瘤相一致,主要发生于55岁以上的患者;(2)胶质母细胞瘤,IDH-突变型(约占10%),近似于临床定义的继发性胶质母细胞瘤,由较低级别弥漫型胶质瘤转化而来,常见于相对年轻的患者;(3)胶质母细胞瘤,NOS,特指那些未能对IDH进行全面评价的胶质母细胞瘤。影像检查可以识别绝大多数的胶质母细胞瘤,尤其是多模式影像检查的联合应用,敏感度最高可达100%,特异度为96%,几乎与组织学诊断一致。
针对新的整合分类,尽管尚没有大样本研究对IDH突变和野生胶质母细胞瘤进行影像比较分析,但IDH突变的胶质母细胞瘤只占少数,约10%,中位发病年龄仅44 岁,较IDH 野生型的62 岁年轻18岁,因此分类相对容易。并且小样本的胶质母细胞瘤的IDH突变型和野生型比较研究已经提示DWI的最小ADC值可以鉴别IDH1(R132H)突变状态。
4. 少突胶质细胞瘤:少突胶质细胞瘤和间变型少突胶质细胞瘤的诊断需要IDH基因突变和1p19q共缺失证实。当基因检测缺失或无确切的基因检测结果时,组织学上典型的少突胶质细胞瘤应归为NOS。针对少突胶质细胞瘤的IDH突变状态的影像检测已经见诸报道。最近的研究提示DTI技术或者DTI 技术联合常规MRI 可以对少突胶质瘤的IDH突变状态做出鉴别,这些发现极大增加了影像检查方法在弥漫型胶质瘤整合诊断的新格局下临床应用的作用。
5. 少突星形细胞瘤:在2016 CNS WHO 肿瘤分类中,少突星形细胞瘤的诊断不再被推荐,而被少突星形细胞瘤,NOS的诊断命名所取代。
6. 儿童弥漫型胶质瘤:新定义一个主要发生在儿童(偶见于成人),以组蛋白H3基因H3F3A或更为少见的相关HIST1H3B 基因K27M 突变为特征的,呈弥漫性生长的中线结构(如丘脑、脑干和脊髓)肿瘤,命名为弥漫型中线胶质瘤,H3 K27M突变。其中就包含了先前提到的弥漫内生型脑桥胶质瘤(DIPG)。针对新的分类,影像检测在儿童弥漫型胶质瘤的术前整合诊断应用几乎未见报道。
7. 髓母细胞瘤:髓母细胞瘤的分类由于联合了组织学表型和分子分型,因而在概念上引起了极大的挑战。该分类不仅包含了临床应用已久的组织学分型(如促纤维组织增生型/结节型、广泛结节型、大细胞型和间变型),还包含了现今被广泛接受的4种基因分型:WNT激活型、SHH激活型、Group3和Group4。这些不同的组织学分型和基因分型在预后和治疗上存在显著差异。该分类并没有采取整合组织学表型与分子分型的联合分类方法,而是利用明确的基因型和组织学定义分别进行分类。希望将来有能力进行分子分型的病理学家能够制定一个既包含组织学分型,又包含分子分型的联合分类方法。这种整合诊断的方法是一种全新的诊断方式,且随着对肿瘤基因型和组织学表型-基因型了解的增加,可能代表一种更为普遍的诊断方法。
随着知识的拓展,这种整合诊断的方法将使肿瘤分型具有更大的弹性。髓母细胞瘤基因分型及影像特征已见诸报道,尽管不同的基因分型的流行病学和组织学特征有所不同,但Perreault等的多中心研究发现影像特征可以预测髓母细胞瘤的基因亚型,这对于临床术前无创识别髓母细胞瘤的基因亚型,改善患者的治疗及预后具有重要的指导意义。SHH激活型(图4~6)在4种髓母细胞瘤基因分型中发病率占第2位,约为30%。组织学类型大多为促纤维增生型/结节型。发病人群多见于婴儿(<4岁)或大多数成人(>16岁)。
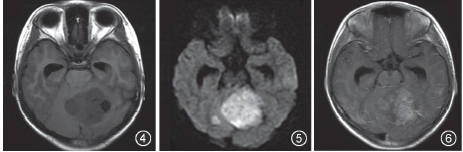
图4~6 女,20 岁,髓母细胞瘤促纤维增生型,SHH 激活型。横断面T1WI(图4)提示左侧小脑半球囊实性占位,呈稍低和低信号,边界清晰;横断面DWI(图5)提示病灶实性部分呈显著高信号;横断面T1WI增强扫描(图6)提示病灶呈明显不均匀斑片状强化
该亚型中54%的肿瘤位于小脑半球,而发生于小脑半球的髓母细胞瘤几乎均为SHH激活型。WNT激活型(图7~9)发病率最低,仅占10%。该基因亚型的髓母细胞瘤90%组织学类型为经典型。发病人群多见于儿童和成人,婴儿罕见。该亚型中75%的肿瘤位于脑桥、小脑或者脑桥小脑角区,发生于上述部位的髓母细胞瘤几乎均为WNT激活型。Group3型(图10~12)发病率占第3位,为20%~25%。与SHH激活型不同,组织学类型大多为经典型或大细胞型/间变型,促纤维增生型/结节型少见。发病人群多见于婴儿和儿童,极少见于青年或成人。
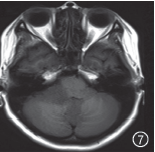
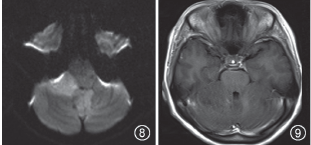
图7~9 女,30岁,髓母细胞瘤经典型,WNT激活型。横断面T1WI(图7)可见小脑下蚓部和右侧桥小脑角区稍低信号占位,边界欠清晰;横断面DWI(图8)显示病灶呈稍高信号;横断面T1WI增强扫描(图9)可见肿瘤区域无明显强化
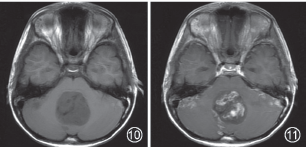

图10~12 男,1岁,髓母细胞瘤经典型,Group3型。横断面T1WI(图10)显示小脑蚓部稍低信号占位,压迫第四脑室,边界清晰,另双侧小脑半球周边可见条片状稍低信号种植灶;横断面和矢状面T1WI增强扫描(图11,12)显示小脑蚓部占位及种植灶表现为不均匀条片状强化
该亚型最容易合并转移,在基因亚型中预后最差;Group4型(图13~15)是4种基因分型中发病率最高的一种亚型,约占35%。除促纤维增生型/结节型外,其他组织学类型在该亚型中均可见。发病人群多见于儿童。该亚型也可发生转移,预后中等。与前两型发病部位不同,Group3和Group4型肿瘤发病部位几乎全部位于中线和第四脑室。Group4型MR增强扫描时肿瘤多数表现为轻度或没有强化,这与Group3型只有极少数有此表现明显不同。因此,根据肿瘤发生部位和强化程度这两个影像学特征可以对大多数髓母细胞瘤的基因亚型做出准确预测。另外,随着高级影像检查模式在髓母细胞瘤应用的逐渐增多,髓母细胞瘤基因亚型的预测准确率有望进一步提高。
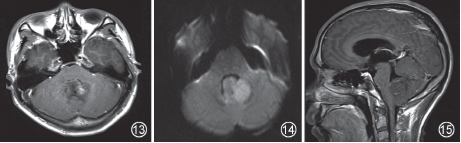
图13~15 男,6岁,髓母细胞瘤间变型/大细胞型,Group4型。横断面T1WI增强扫描(图13)显示小脑下蚓部占位病灶,占据第四脑室,肿瘤可见少许小片状强化;横断面DWI(图14)显示病灶呈稍高信号;矢状面T1WI增强扫描(图15)显示肿瘤实质少许强化,压迫下部第四脑室
8. 其他胚胎源性肿瘤:髓母细胞瘤以外的胚胎源性肿瘤在分型上也有重要改变,原始神经外胚层肿瘤(primitive neuroectodermal tumor, PNET)被从诊断词条中删除。非典型畸胎样/横纹肌样瘤(atypical teratoid/rhabdoid tumor,AT/RT)现在以INI1 或者非常罕见的BRG1 突变来定义,所以今后AT/RT的诊断需要明确的特征性分子检测。随着PNET在新分类词条中被删除,对髓母细胞瘤以外的胚胎源性肿瘤影像特征也亟待重新整理。尤其是需要紧密结合新分类中C19MC基因扩增的情况,对多层菊形团样胚胎源性肿瘤(embryonal tumors with multilayered rosettes,ETMR)的影像特征进行重新归类。然而,关于ETMR影像特征的总结报道样本较少,自2000至2015年间全世界ETMR报道不足100例,影像特征总结就更少。通过对100例病例的回顾性分析显示,已经有一些发病特征对于ETMR的识别具有重要的参考价值,如ETMR主要见于小年龄组儿童(平均2岁左右),65%发病于幕上,额叶和顶叶多见,主要累及皮层;35%发生于幕下。另外,少部分ETMR肿瘤可侵犯硬脑膜,早期即可有脊髓转移,甚至一开始就以脊髓受累发病。
9. 其他CNS肿瘤:间变型多形性黄色星形细胞瘤,WHO Ⅲ级,作为一个明确分型加入2016 CNSWHO肿瘤分类。毛细胞黏液样星形细胞瘤的分级也发生了改变,新分类建议降低毛细胞黏液样星形细胞瘤的分级。神经鞘瘤和脑膜瘤均变化不大。孤立性纤维性肿瘤/血管外皮瘤,作为一个全新的诊断,将原来低级别的孤立性纤维瘤和原来高级别的血管外皮细胞瘤及间变型血管外皮细胞瘤均包括在内;孤立性纤维瘤/血管外皮细胞瘤具有共同的分子特征。
室管膜瘤,RELA融合基因阳性,作为一个全新的由基因定义的室管膜瘤亚型加入2016 CNS WHO肿瘤分类,该亚型在儿童幕上肿瘤尤为多见。神经元与混合型神经元-胶质肿瘤中新增弥漫型软脑膜胶质神经元肿瘤的命名,该类型患者预后多变,肿瘤生长缓慢,往往容易继发脑积水。淋巴瘤和组织细胞性肿瘤分类与血液淋巴系统WHO分类保持一致。对于上述CNS肿瘤分类的变化,尤其是对那些整合了基因诊断的新病种尚缺乏影像学特征的总结。这些新病种是否具有特征性的影像形态学表征,或者在反映肿瘤功能、代谢和分子水平层面,先进的影像检测方法是否能够发现特征性生物标记指向肿瘤基因突变,对新分类下帮助临床制定个体化治疗方案和改善患者预后均具有重要的意义。
三、影像医学
在分子病理时代面临的挑战2016 CNS WHO 肿瘤分类相比2007版的一个明显进步是首次将分子信息应用于脑肿瘤诊断。这给命名法、疾病分类学和报告结构提出挑战,同时下一版的CNS WHO肿瘤分类在分型中将整合入更客观的分子信息,而当前版本可能只作为过渡阶段。此外,因为该分类留下一些NOS类别的分类,允许更多研究集中在这些未明确定义的分组从而最终确定这些分型。该分型在许多情况下能够在缺乏分子数据时进行诊断,并进行了明确的分类,而且允许分子分型组和无分子分型组同时存在。从长远考虑,2016 CNS WHO肿瘤分类将进一步促进临床、实验室和流行病学的研究,最终改善脑肿瘤患者的生存。
2015年1月20日,美国总统奥巴马在国情咨文演讲中提到了“精确医疗计划”,从而拉开了精准医疗的帷幕,精准医疗的概念自此受到全世界的关注。传统的以形态诊断为主的影像医学模式显然无法承担起这个使命,它所提供的形态学表现已远远不能满足精准医疗所需要的分子与基因水平的生物学信息。现代成像工具和成像生物标志物可以用来定义某些疾病的特征性个体化的影像学表型,也为提供类似预测疾病预后、模拟治疗方法、评估治疗反应奠定了基础。
今天的影像医学整合了反映功能、代谢和分子水平信息的现代影像学技术,提供患者个体化诊断信息的能力大大增强。但是2016 CNS WHO 肿瘤新分类给影像医学提出了巨大的挑战。我们能不能应对这样的挑战?能不能在无创的体内诊断中继续扛起领导的大旗?为了适应这样的挑战,传统的影像医学诊断模式亟待改变,影像医学必须与分子生物学、分子病理学结合,必须与新型治疗模式、预后判断和康复结合,打破学科壁垒,促进各种影像技术的融合,以新的角度来重新考虑影像医学的发展。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#神经系统肿瘤#
47
学到了很多,谢谢!
80
好东西大家一起学!
51
学习到了,很好
63
很好,不错,以后会多学习
86
很好,不错,以后会多学习
55
增加分子分型来对CNS肿瘤进行定义
25
很好,不错,以后会多学习
28
不错!
39
#神经系统#
50