Cardiovasc Diabetol:在2型糖尿病患者中,hs-CRP是心血管事件和全因死亡率的危险因素
2021-11-20 MedSci原创 MedSci原创
慢性低度炎症可能是降低2型糖尿病患者心血管风险的治疗目标。
心血管疾病是2型糖尿病患者住院和死亡的主要原因。与非2型糖尿病患者相比,2型糖尿病患者心血管疾病发病率和死亡率较高。大多数观察到的心血管风险增加归因于已知心血管危险因素的聚集(如高血压、血脂异常和高血糖),但即使按照国际心血管预防指南进行治疗,仍然存在大量的残余心血管风险,低级别炎症可能发挥重要作用。
高敏CRP (hs-CRP)是全身低级别炎症的标志,在不同人群中较高的血浆水平与心血管事件相关。本研究的目的是评估hs-CRP与高危2型糖尿病患者心血管事件发生率和全因死亡率之间的关系。
本研究纳入1679名2型糖尿病患者,采用Cox比例危险模型评估hs-CRP对心血管事件(心肌梗死、卒中和血管死亡的复合)和全因死亡的风险。Hs-CRP进行对数转化以进行连续分析。根据年龄、性别、BMI、当前吸烟和饮酒、非hdl -胆固醇和微量蛋白尿对研究结果进行了调整。
中位随访时间为7.8年,可以看到共发生307例新的心血管事件和343例死亡(IQR 4.2-11.1)。与第一个三分位患者相比,第三个三分位患者的死亡风险高89%。与第一个三分位患者相比,第三个三分位患者的血管死亡风险也增加(HR 1.87,95%CI 1.22–2.85)。
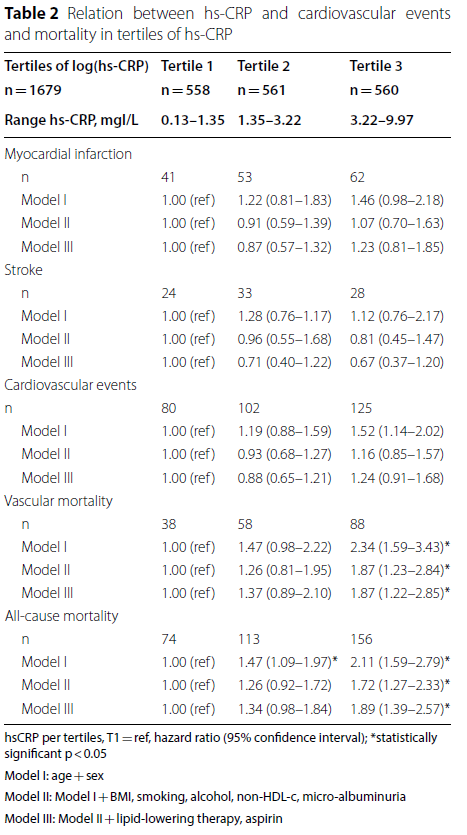
hs-CRP与hs-CRP组心血管事件和死亡率的关系
持续分析时,对数(hs-CRP)增加一个单位与死亡率风险增加相关(HR 1.26,95%可信区间1.10–1.45)。log(hs-CRP)增加一个单位也与血管死亡率风险增加相关(HR 1.21,95%可信区间1.01–1.46)。亚组分析不支持存在明显血管疾病的效应调整(所有相互作用的p值均>0.05)此外,降脂治疗和阿司匹林使用的额外调整并未改变结果。
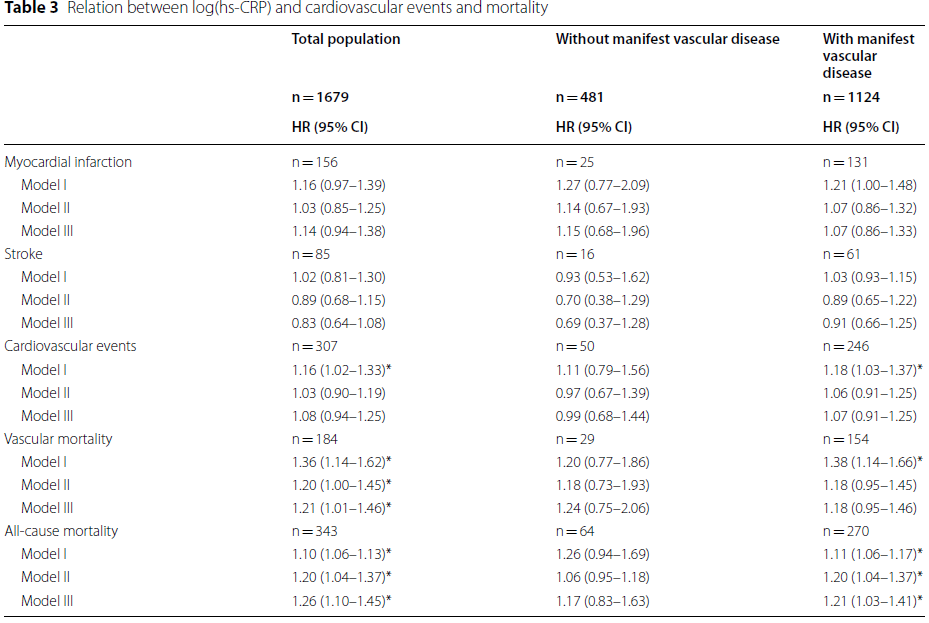
log(hs-CRP)与心血管事件和死亡率的关系
总的来说, hs-CRP测量的低度炎症是2型糖尿病高危患者血管和全因死亡率的独立危险因素,但不是心血管事件的独立危险因素。慢性低度炎症可能是降低2型糖尿病患者心血管风险的治疗目标。
参考文献:Sharif, S., Van der Graaf, Y., Cramer, M.J. et al. Low-grade inflammation as a risk factor for cardiovascular events and all-cause mortality in patients with type 2 diabetes. Cardiovasc Diabetol 20, 220 (2021). https://doi.org/10.1186/s12933-021-01409-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ASC#
31
#DIA#
33
#BET#
28
#血管事件#
26
#全因死亡率#
46
#CRP#
54
#2型糖尿病患者#
24
#糖尿病患者#
26
#hs-CRP#
27
学习
35