JAMA Surg:多重干预措施用于普外科及骨科高龄患者术后谵妄的预防
2021-12-21 MedSci原创 MedSci原创
多方面的预防干预措施可显著降低骨科以及普外科老年患者术后谵妄风险

老年患者术后谵妄风险较高,导致术后死亡率增加,认知能力和自理能力下降,住院治疗和费用支出增加。随着人口老龄化加剧,预防老年患者术后谵妄十分必要。研究称,约三分之一的术后谵妄病例是可预防的,且不需要药物干预。近日研究人员考察了多方面的预防干预措施对降低大手术后谵妄风险的作用。

研究在德国开展,总计招募了1470名70岁以上老年患者,患者择期进行骨科、普外或心脏外科手术。首先,向每个临床中心的护理人员提供了结构化的谵妄教育,预防小组每天评估患者谵妄危险因素和症状。预防方案是根据患者个体化定制的,包括:认知、运动和感觉刺激、饮食陪伴、诊断过程中压力放松和睡眠促进。研究的主要终点为术后谵妄。
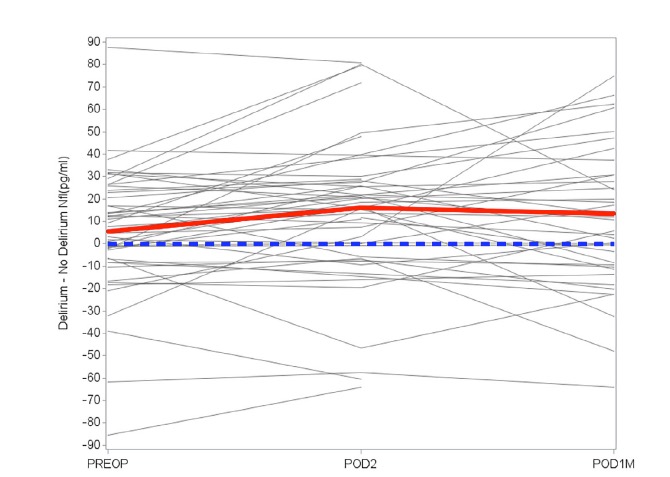
参与者中男性763人(51.9%),平均年龄77岁。总体上,干预措施可有效降低谵妄事件(OR=0.87)风险以及谵妄天数百分比(干预组 vs 对照组=5.3% vs 6.9%)。骨科以及普外科(OR=0.59)患者从干预中获益显著,但心脏外科(1.18)的效果不显著。
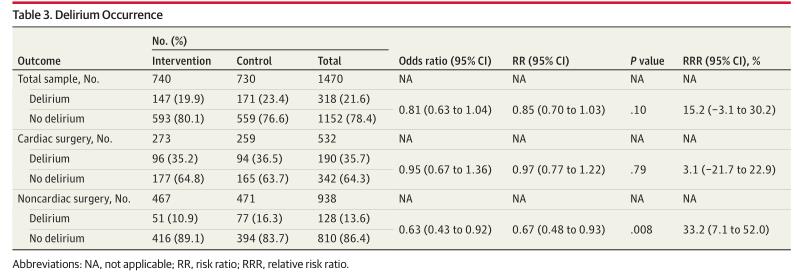
多重干预对术后谵妄风险的影响
研究发现,多方面的预防干预措施可显著降低骨科以及普外科老年患者术后谵妄风险。
原始出处:
Friederike Deeken et al. Outcomes of a Delirium Prevention Program in Older Persons After Elective Surgery A Stepped-Wedge Cluster Randomized Clinical Trial. JAMA Surg,December 15,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#干预措施#
51
#高龄患者#
35
不错
44
#术后谵妄#
47
#高龄#
48
一篇论文中,研究团队对在检疫酒店
57
不错学习了。
69