Hypertension:AT2R通过抑制Kir4.1调控NCC和肾脏的泌K+功能
2018-03-03 MedSci MedSci原创
AT2R(血管紧张素II 2型受体)表达于远端肾单位。研究人员进行实验探究AT2R是否可调节远曲小管NCC(Na-Cl协同转移体)和Kir4.1的表达。用氯沙坦治疗时,血管紧张素II(AngII)可抑制远曲小管基底外侧膜的40pS K+通道(Kir4.1/5.1异质四聚体),但用PD123319治疗时,无相似现象。AT2R兴奋剂也可抑制K+通道,提示AT2R参与Kir4.1的主要调控。输注PD12
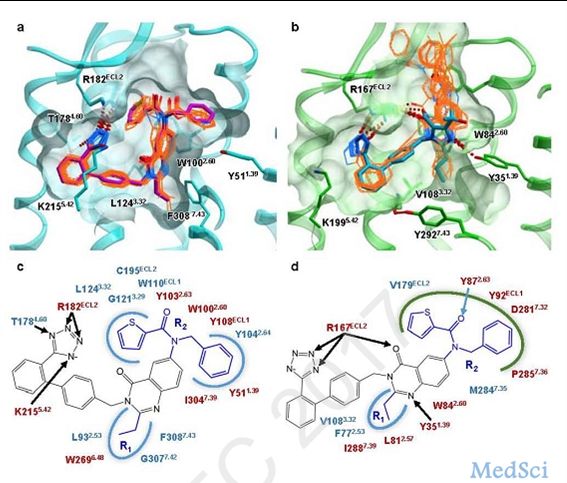
AT2R(血管紧张素II 2型受体)表达于远端肾单位。研究人员进行实验探究AT2R是否可调节远曲小管NCC(Na-Cl协同转移体)和Kir4.1的表达。
用氯沙坦治疗时,血管紧张素II(AngII)可抑制远曲小管基底外侧膜的40pS K+通道(Kir4.1/5.1异质四聚体),但用PD123319治疗时,无相似现象。AT2R兴奋剂也可抑制K+通道,提示AT2R参与Kir4.1的主要调控。输注PD123319的4天内,可通过时间依赖性方式,刺激tNCC(总NCC)和pNCC(磷酸化的NCC;Thr53)的表达。PD123319治疗4天,可刺活基地外侧膜的40pS K通道,增强基地膜外侧的K+电导,从而增加远曲小管膜的负值。研究人员发现只有在野生型小鼠中抑制AT2R可增强tNCC和pNCC的表达,而在肾脏特异性敲除Kir4.1的小鼠中,没有相同的现象,因此推测激活Kir4.1对PD123319诱导的NCC增强至关重要。肾清除研究显示,用PD123319处理小鼠4天时,噻嗪类(利尿药)诱导的排钠效应会明显增强(与未用PD123319处理的小鼠相比)。但在特异性敲除肾Kir4.1的小鼠中观察不到该效应。最后,AT2R拮抗剂可降低野生型小鼠肾脏的排K功能,引发高血压,而在特异性敲除肾脏Kir4.1的小鼠中则不会。
总而言之,AT2R依赖性的NCC调控,需要远曲小管的Kir4.1的参与,AT2R通过抑制Kir4.1和NCC来刺激K+分泌。
原始出处:
Peng Wu, et al.AT2R (Angiotensin II Type 2 Receptor)-Mediated Regulation of NCC (Na-Cl Cotransporter) and Renal K Excretion Depends on the K Channel, Kir4.1.Hypertension. February 26,2018. https://doi.org/10.1161/HYPERTENSIONAHA.117.10471
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#PE#
23
#TENS#
23
#Hypertension#
24
学习了.获益匪浅.感谢分享
41