Heart:ICD置入者临床转归存在性别差异
2013-06-04 高晓方 译 医学论坛网
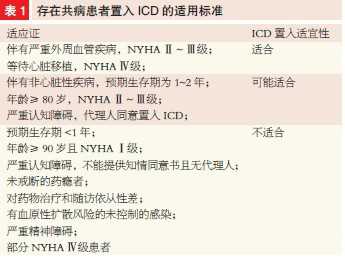
荷兰一项研究表明,与男性相比,置入型心律转复除颤器(ICD)女性置入者的死亡率较低,并且适当ICD治疗倾向于较少。论文于5月30日在线发表于《心脏》(Heart)。 此项研究前瞻性人群研究共纳入1946例一级预防ICD置入患者,其中男、女性分别占79%和21%。主要转归指标为全因死亡、ICD治疗(抗心动过速起搏和电击)以及ICD电击。 结果显示,在中位随访3.3年期间,
荷兰一项研究表明,与男性相比,置入型心律转复除颤器(ICD)女性置入者的死亡率较低,并且适当ICD治疗倾向于较少。论文于5月30日在线发表于《心脏》(Heart)。
此项研究前瞻性人群研究共纳入1946例一级预防ICD置入患者,其中男、女性分别占79%和21%。主要转归指标为全因死亡、ICD治疗(抗心动过速起搏和电击)以及ICD电击。
结果显示,在中位随访3.3年期间,男、女性分别有387例(25%)和76例(18%)死亡。男、女性估计5年累积全因死亡率分别为20%和14%。对潜在混淆协变量进行校正之后,女性的全因死亡率较低(HR 0.65;P<0.01)。男、女性5年估计累积适当治疗发生率分别为24%和20%。校正之后非显著趋势依然存在。

Objective
To assess differences in clinical outcome of implantable cardioverter-defibrillator (ICD) treatment in men and women.
Design
Prospective cohort study.
Setting
University Medical Center.
Patients
1946 primary prevention ICD recipients (1528 (79%) men and 418 (21%) women). Patients with congenital heart disease were excluded for this analysis.
Main outcome measures
All-cause mortality, ICD therapy (antitachycardia pacing and shock) and ICD shock.
Results
During a median follow-up of 3.3 years (25th–75th percentile 1.4–5.4), 387 (25%) men and 76 (18%) women died. The estimated 5-year cumulative incidence for all-cause mortality was 20% (95% CI 18% to 23%) for men and 14% (95% CI 9% to 19%) for women (log rank p<0.01). After adjustment for potential confounding covariates all-cause mortality was lower in women (HR 0.65; 95% CI 0.49 to 0.84; p<0.01). The 5-year cumulative incidence for appropriate therapy in men was 24% (95% CI 21% to 28%) as compared with 20% (95% CI 14% to 26%) in women (log rank p=0.07). After adjustment, a non-significant trend remained (HR 0.82; 95% CI 0.64 to 1.06; p=0.13).
Conclusions
In clinical practice, 21% of primary prevention ICD recipients are women. Women have lower mortality and tend to experience less appropriate ICD therapy as compared with their male peers.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#ICD#
24
#临床转归#
45
#ART#
33
#HEART#
32