术式创新!肋软骨弹簧移植矫正成人唇裂鼻畸形
2021-12-28 MedSci原创 MedSci原创
因为软骨的脆弱性和紧密收缩的软组织易塌陷,唇裂鼻畸形的后期矫正仍然是一个挑战。作者描述了肋骨软骨弹簧移植的新技术,将鼻小柱和下外侧软骨作为一块,用于唇裂鼻畸形的后期矫正,以获得对称、美观、更持久和可接
因为软骨的脆弱性和紧密收缩的软组织易塌陷,唇裂鼻畸形的后期矫正仍然是一个挑战。作者描述了肋骨软骨弹簧移植的新技术,将鼻小柱和下外侧软骨作为一块,用于唇裂鼻畸形的后期矫正,以获得对称、美观、更持久和可接受的结果。
图1 文章来源
该研究团队对92例单侧唇裂鼻畸形患者行晚期唇裂鼻修复同期鼻整形术。为了矫正唇裂鼻畸形,用肋软骨(自体或同种异体)制备了宽度为2至3 mm、厚度为0.5至1 mm、长度为5至7 cm的支撑移植物。
用手指使支撑移植物弯曲,来模拟鼻翼软骨的内侧和外侧脚。从鼻翼缘做新月形皮肤切口,并在小柱处进行垂直切口。解剖鼻翼区,为弓形弹簧软骨移植物的植入创造足够的空间。
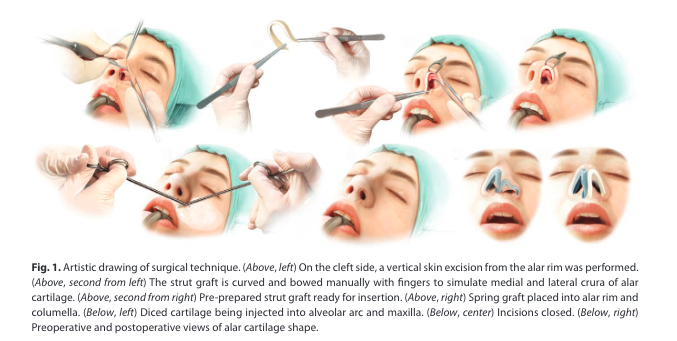
图2(上图,左)在裂侧,从鼻翼缘进行垂直皮肤切除。(上图,左二)用手指手动弯曲支撑移植物,以模拟鼻翼软骨的内侧和外侧脚。(上图,右二)预先准备好的支架移植物,准备插入。(右上)弹簧移植物植入鼻翼缘和小柱。(下图,左)将切好的软骨注射到牙槽弧和上颌骨中。(下方,中间)切口闭合。(右下)鼻翼软骨形状的术前和术后视图

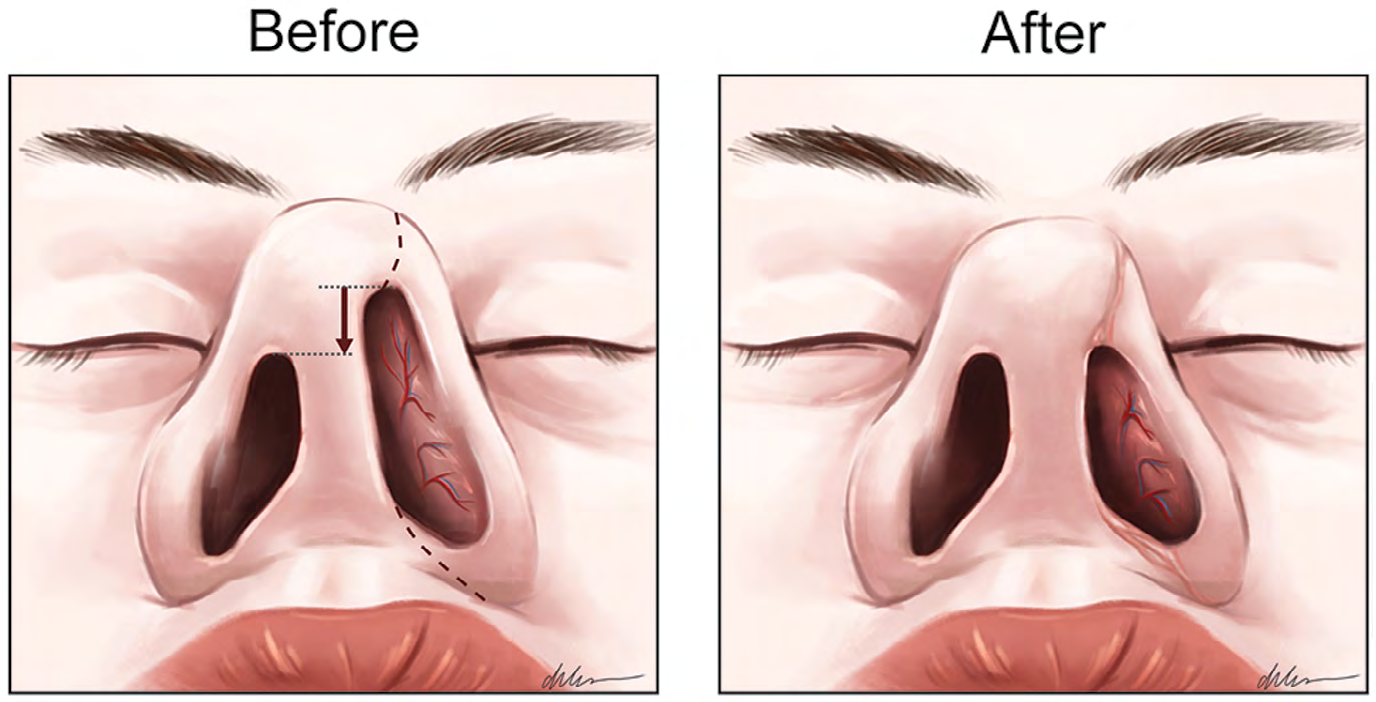
图3通过上唇沟注射切成小块的软骨,以增加凹陷的上颌骨弧。
植入软骨移植物后,鼻翼缘用连续6-0Monocryl可吸收线缝合,鼻小柱用5-0可吸收线缝合。
所有病例均矫正了鼻翼软骨畸形和唇腭裂,使用弹簧肋软骨延长了鼻小柱,鼻孔对称。平均随访时间为9年(范围为1至15年)。结果从好到好。几年后,所有患者都保留了较好的正中脚和外侧脚的形状和对称性,在触诊过程中,移植物对手指压力的抵抗力得到了提高。在10%的患者(n=9)中,在1年随访结束时仅进行了轻微的修补手术。在所有患者中,肋骨弹簧移植物保留了其形状和结构。
因此,在自体和异体移植物之间没有发现差异。由于肋软骨弹簧移植物的插入,也没有出现伤口裂开。在接受自体肋软骨移植的患者中,没有发生供区并发症。
用单侧或双侧分叉皮瓣延长小柱,从鼻翼边缘切除新月形物,插入肋软骨弹簧支柱作为弓矫正鼻翼凹陷,用软骨碎片塑造尖端,用肋软骨碎片注射增加牙槽和上颌弓,鼻翼底部楔形切除、鼻中隔成形术和同期鼻成形术提供了一致、持久的满意结果。弹簧肋软骨支柱模拟了下外侧软骨的内侧脚和外侧脚的形状,可在几年内保护其形状和硬度。
这些手术、鼻中隔成形术和同期鼻整形术为唇裂鼻畸形的后期矫正提供了长期满意的结果。
原始文章:
Erol Onur O,Agaoglu Galip,Costal Cartilage Spring Graft for Late Correction of Cleft Lip Nose Deformity: New Technique.[J] .Plast Reconstr Surg, 2021, 148: 983e-991e.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#肋软骨#
37
#鼻畸形#
35
#创新#
35
#畸形#
42