Am J Med:大脑之窗:眼科护士的神经眼科知识!
2017-11-15 cuiguizhong MedSci原创
Prasad S近日在Am J Med杂志上发表了一篇文章,题目是"A Window to the Brain: Neuro-Ophthalmology for the Primary Care Practitioner",详细介绍了视觉症状与重要神经疾病的关系,提出初级眼科临床护士应该具备对这些征兆进行适当的初步诊断的能力。
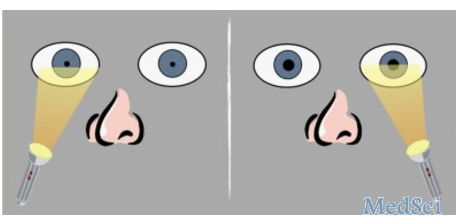
Prasad S近日在Am J Med杂志上发表了一篇文章,题目是"A Window to the Brain: Neuro-Ophthalmology for the Primary Care Practitioner",详细介绍了视觉症状与重要神经疾病的关系,提出初级眼科临床护士应该具备对这些征兆进行适当的初步诊断的能力。视觉症状可能是广泛的重要神经疾病的征兆特征。这些视觉征兆包括急性单眼视力丧失、视神经乳头水肿、视野缺陷、瞳孔大小不等、眼睛运动受限和眼球震颤等。对于初级眼科临床护士来说,重要的是要能够对这些征兆进行适当的初步诊断,并根据诊断结果提出治疗和转诊等措施。例如上图是单侧视神经病变的特征是相对传入性瞳孔缺损(RAPD)-左相对传入瞳孔缺损示意图。光源来回摆动。当光照射到右眼时,瞳孔都收缩。当光源照射到左眼时,瞳孔都膨胀。原文出处:Prasad, S., A Window to the Brain: Neuro-Ophthalmology for the Primary Care Practitioner. Am J Med, 2017.本文系梅斯医学(MedSci)原创编
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Med#
32
不错的文章值得推荐
69
非常好的文章.学习了
74
看看
66