合理制定靶向药物使用顺序,使mCRC患者获益很大化
2017-07-19 陈治宇 中国医学论坛报
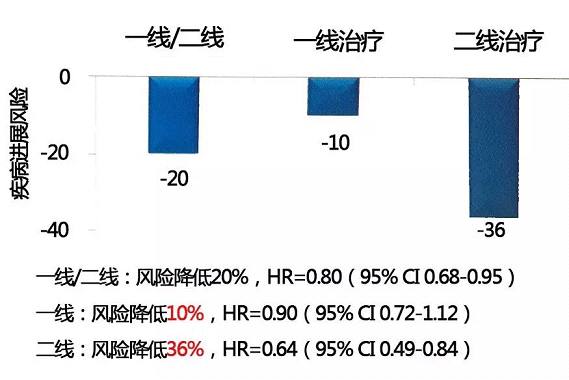
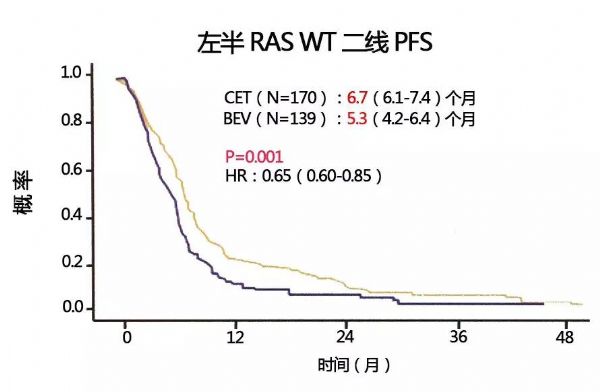
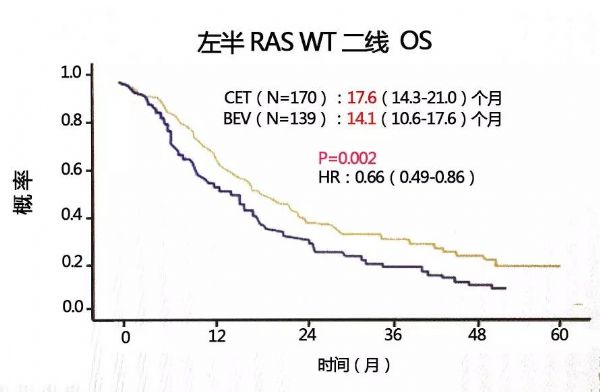
回顾临床前研究数据显示,肿瘤细胞发生获得性抗-EGFR单抗耐药后,VEGF的表达及释放均上升。因此,既往曾接受抗-EGFR单抗治疗的肿瘤细胞可能对抗-VEGF单抗的治疗更为敏感。那么一线接受化疗联合抗-EGFR单抗治疗的mCRC患者,二线换用含贝伐珠单抗治疗方案会取得更优的疗效表现吗?抑或一线接受化疗联合贝伐珠单抗,二线换用含抗EGFR单抗方案更优?近年ASCO及ASCO GI上公布的研究探讨了这
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#mCRC#
30
#药物使用#
24
#CRC#
18
学习谢谢分享!
65
感谢小编为我们精心准备了如此精辟的精神大餐,小编辛苦了,点个赞吧!
63
学习了分享了
45