J Gastroenterol Hepatol:在流行地区对胆管癌的超声监测提供了生存的好处
2018-01-28 MedSci MedSci原创
腹部超声使生存获益;在高度流行地区,腹部超声应该被考虑,以降低CCA死亡率。
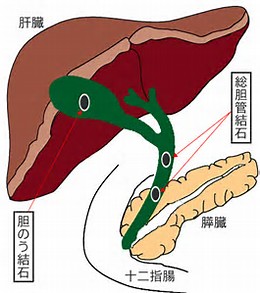
胆管癌(CCA)是一种恶性肿瘤,进展迅速,预后差。腹部超音监测可检测早期恶性肿瘤并改善手术结果。然而,在流行地区CCA发展的高危人群中,腹部超声监测的相关数据却很少。本研究比较了通过腹部超声监测项目招募的CCA患者的生存状况,以及对住院患者的生存率。
该监测人群为泰国北部的4225名村民,年龄在30-60岁之间,他们同意接受为期5年的腹部超声监测计划,每6个月进行一次间隔超声检查。非监测队列是2007年4月至2015年11月被医院诊断为CCA的患者。比较监测组和未监测组患者的可手术性肿瘤、R0切除百分比和生存分析。
在监测和非监测组中分别有48名和192名CCA患者。在这些CCA患者中,37/48(77.1%)和22/192(11.5%)的患者处于手术可操作阶段;两组研究队列患者R0切除率分别是36/48(97.3%)和14/192(63.6%)。各组中位存活期分别为31.8个月和6.7个月(P<0.0001)。多元分析表明,腹部超声检测(HR=0.41; p=0.012),手术可操作阶段(HR=0.11; p<0.001),血清白蛋白≥3.5 g/dL(HR=0.42; p<0.001)与死亡率降低独立相关;然而,CAA肿瘤大小(HR=1.11; p<0.001),血清ALT> 40 IU/L (HR=1.71; p=0.017)和肿瘤再复发(HR=4.86; p=0.017)与死亡率增加显著相关。
腹部超声使生存获益;在高度流行地区,腹部超声应该被考虑,以降低CCA死亡率。
原始出处
Siripongsakun S, Vidhyarkorn S, Charuswattanakul S, et al. Ultrasound Surveillance for Cholangiocarcinoma in an Endemic Area Provided Survival Benefits. J Gastroenterol Hepatol, 2017, Dec 16. doi: 10.1111/jgh.14074.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Gastroenterol#
17
#GAS#
34
#AST#
28
#EPA#
22
#胆管#
23