JAMA:恶性贫血-案例报道
2016-05-09 Mechront 译 MedSci原创
患者女,25岁,疲劳、体重下降3周。既往有缺铁性贫血和甲状腺功能减退症。近期患者因甲状腺功能减退症入院,辅助检查:TSH 209.1 µIU/mL (0.4-4.0 µIU/mL),游离甲状腺素 0.4 ng/dL (0.7-1.5 ng/dL),WBC 3800/µL,PLT 158 ×103/L,Hb 6.9 g/dL,MCV 107 μm3。患者开始服用左旋甲状腺素钠片,此外没有
患者女,25岁,疲劳、体重下降3周。
既往有缺铁性贫血和甲状腺功能减退症。
近期患者因甲状腺功能减退症入院,辅助检查:TSH 209.1 µIU/mL (0.4-4.0 µIU/mL),游离甲状腺素 0.4 ng/dL (0.7-1.5 ng/dL),WBC 3800/µL,PLT 158 ×103/L,Hb 6.9 g/dL,MCV 107 μm3。患者开始服用左旋甲状腺素钠片,此外没有服用其他药物。
此次就诊患者生命体征和查体均未见明显异常。辅助检查:TSH 31.4 µIU/mL,游离甲状腺素 0.7 ng/dL,WBC 2600/µL,PLT 86 ×103µL,Hb 6.3 g/dL,网织红细胞计数 3.1%,MCV 106 μm3,LDH 3116 U/L(0-271),结合珠蛋白
< 8 mg/dL(30-200),维生素B12 1313 pg/mL (200-933),叶酸 > 25 ng/mL(>5.9)。外周血涂片和骨髓活组织检查分别见图A和B。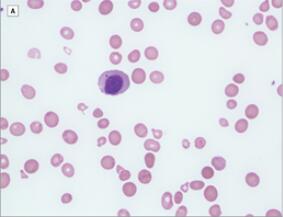
图A:外周血涂片可见小红细胞、巨红血球、泪滴细胞,中性粒细胞减少和血小板减少;有核细胞的中心是一个含有Howell-Jolly小体(染色质小体)的骨髓巨幼红细胞。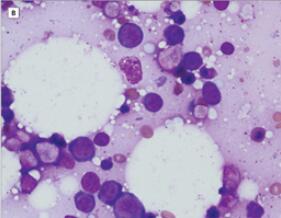
图B:骨髓活检显示红系明显增生伴巨幼红细胞变化,包括异步核、胞质成熟、核出芽和多核。
诊断:恶性贫血。
接着查患者血清MMA为2.33 μmol/L (<0.40),且内因子抗体检测呈阳性。
治疗:联合肠外和口服维生素B12替代治疗。
患者的临床症状渐得到改善。2个月后辅助检查:Hb 11.0 g/dL,WBC 4.2 K/μL,PLT 366 K/μL,MCV 78 fL,LDH在正常范围内。患者继续口服维生素B12和左旋甲状腺素钠片。
在美国恶性贫血发生率约为50/100 000 - 400/100 000,是维生素B12缺乏症最常见的原因。恶性贫血与其他自身免疫性疾病相关,包括Graves病和1型糖尿病,此外,在欧洲北部和非洲血统的人中,恶性贫血在老年人中更常见。
维生素B12对正常造血细胞的成熟是必不可少的。骨髓中红细胞成熟障碍会导致巨幼红细胞性贫血;严重不足时,白细胞和巨核细胞破坏髓内溶血导致高LDH水平、低蛋白水平和全血细胞减少。一般对恶性贫血的治疗采用肌注维生素B12,因为口服效果疗效慢。
原始出处:
McMahon B, Kamath S,Pancytopenia in a Patient With Hypothyroidism.JAMA. 2016 Apr 19;315(15):1648-9. doi: 10.1001/jama.2016.2155.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#恶性贫血#
30
很不错的
134
值得学习
134
同问,这样也可以作为个案报道?
121
这样也行?
176
值得阅读,学习!
120