Thorax:抗血小板治疗可降COPD急性加重期患者死亡?
2014-04-24 小田 译 医学论坛网
有研究表明,慢性阻塞性肺疾病急性加重期(AECOPD)患者的血小板活性增加。系统炎症与COPD患者短期和长期转归差有关。英国学者对血小板增多症是否与AECOPD转归差具有独立相关性进行了探索,结果表明,在校正混淆因素后,血小板增多与COPD加重后1年死亡率增加具有相关性。抗血小板治疗可显著降低AECOPD患者的1年死亡率,并且可能有保护性作用。研究论文4月17日在线发表于《胸》(Thorax)杂志
有研究表明,慢性阻塞性肺疾病急性加重期(AECOPD)患者的血小板活性增加。系统炎症与COPD患者短期和长期转归差有关。英国学者对血小板增多症是否与AECOPD转归差具有独立相关性进行了探索,结果表明,在校正混淆因素后,血小板增多与COPD加重后1年死亡率增加具有相关性。抗血小板治疗可显著降低AECOPD患者的1年死亡率,并且可能有保护性作用。研究论文4月17日在线发表于《胸》(Thorax)杂志。
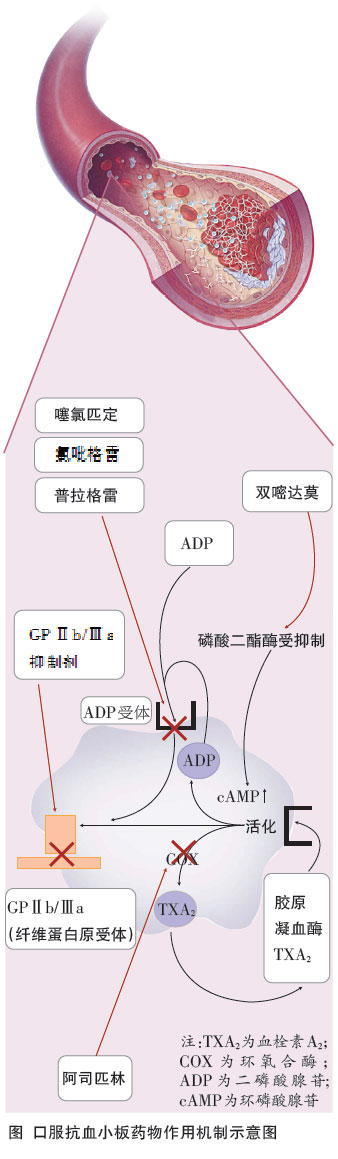
结果显示,157例(11.7%)患者有血小板增多症。血小板增多症与患者1年死亡和院内死亡均具有相关性(OR 分别为1.53和2.37)。在伴有血小板增多症的患者中,心血管住院并未显著增加(OR 1.13)。阿司匹林或氯吡格雷治疗与1年死亡率减少具有相关性(OR 0.63,P=0.003),但与院内死亡无相关性(OR 0.69 ,P=0.124)。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










好的,好文章
146
#急性加重#
33
#患者死亡#
31
#急性加重期#
25