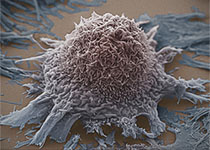
CLIN CANCER RES:肿瘤切除可以募集效应T细胞并增强胶质瘤干细胞疗效
2017-11-28 MedSci MedSci原创
尽管肿瘤切除是胶质瘤一线的临床治疗方式,但是有很多临床前免疫治疗模型进行胶质瘤治疗的研究。减瘤手术诱导的免疫反应联合免疫因子输入为胶质瘤免疫治疗提供了一种新的治疗模式。CLIN CANCER RES近期发表了一篇文章研究这一问题。
尽管肿瘤切除是胶质瘤一线的临床治疗方式,但是有很多临床前免疫治疗模型进行胶质瘤治疗的研究。减瘤手术诱导的免疫反应联合免疫因子输入为胶质瘤免疫治疗提供了一种新的治疗模式。CLIN CANCER RES近期发表了一篇文章研究这一问题。作者建立了肿瘤切除原位胶质瘤鼠模型,研究肿瘤切除的免疫反应。作者还建立了大量分泌免疫因子IFNβ的工程化鼠间充质干细胞(MSC-IFNβ)并评估颅内胶质瘤肿瘤切除是否可以显着增强MSC-IFNβ的抗肿瘤活性。研究结果表明,减瘤后髓系抑制性细胞(MDSC)持续减少并刺激CD4/CD8T细胞募集。这一免疫反应可以通过增强术后CD8T细胞浸润以及直接诱导肿瘤细胞细胞周期阻滞显着增强MSC-IFNβ的抗肿瘤活性,最终延长鼠的生存。利用人胶质瘤肿瘤异种移植原位切除模型,作者发现IFNβ可以诱导细胞周期阻滞使细胞凋亡,从而延长免疫缺陷鼠的生存时间,尽管这些老鼠缺乏完整的免疫系统。文章最后认为,该研究证明了原位肿瘤切除模型在肿瘤免疫治疗发展中的重要作用,局部输入免疫治疗性药物治疗肿瘤具有转化潜力。原始出处:Sung Hugh Choi,Daniel W.Stuckey,et
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#胶质瘤干细胞#
29
#肿瘤切除#
52
值得进一步研究
64
不错的.学习了!谢谢分享!
72
学习
60