Geroscience:MT和炎症与有合并症的老年人较差的身体功能密切相关
2020-10-02 MedSci原创 MedSci原创
据推测,肠道屏障功能障碍是导致衰老的两个显著特征(炎症和身体机能下降)的决定因素。据报道,在健康的老年人、大鼠和无脊椎动物中,微生物转位(MT)或其生物标志物(脂多糖结合蛋白-1[LBP-1]、可溶性
据推测,肠道屏障功能障碍是导致衰老的两个显著特征(炎症和身体机能下降)的决定因素。据报道,在健康的老年人、大鼠和无脊椎动物中,微生物转位(MT)或其生物标志物(脂多糖结合蛋白-1[LBP-1]、可溶性分化簇[sCD]-14)与身体功能之间存在关联。然而,尚不清楚是否存在合并症,或旨在通过减肥或运动减少合并症的临床干预措施会改变这种联系,研究结果已在线发表于Geroscience。
研究人员测量了288名超重/肥胖的老年患者的炎症、MT和身体功能,这些患者患有心脏代谢疾病和自我报告的行动限制,参加了减肥和生活方式干预研究。
结果显示,基线时期,校正年龄、性别和体重指数后,炎症细胞因子和LBP-1呈正相关。校正协变量后,较高的LBP-1与较差的身体功能密切相关。此外,即使IL-6水平被纳入模型,400米步行时间(p = 0.003)、短体能表现(p = 0.07)和IL-8(p <0.001)仍然与LBP-1正相关。生活方式干预改善了身体质量和一些功能测量;然而,MT和炎症没有变化。
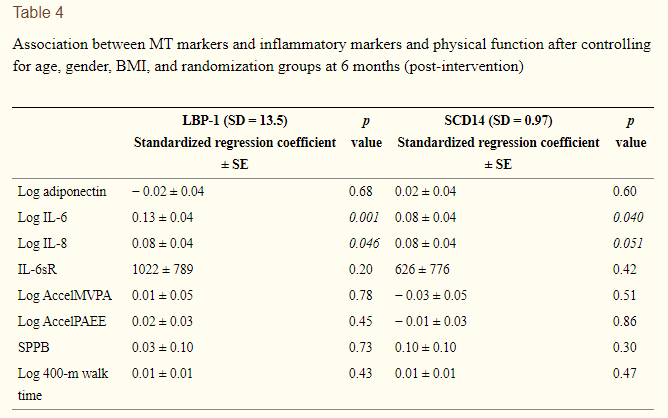
综上所述,该研究结果表明,MT与炎症以及有合并症的老年人较差的身体功能密切相关。肠道屏障功能似乎并没有因为干预措施的分配而得到改善,这表明需要采取其他策略来针对衰老中的这种促炎途径。
原始出处:
Kylie Kavanagh, Fang-Chi Hsu, et al., Biomarkers of leaky gut are related to inflammation and reduced physical function in older adults with cardiometabolic disease and mobility limitations. Geroscience. 2019 Dec;41(6):923-933. doi: 10.1007/s11357-019-00112-z.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#合并症#
25
#GER#
37
#ROS#
27
#SCIE#
21