NEJM:下腔静脉滤器支柱栓塞-病例报道
2018-04-12 xing.T MedSci原创
该患者经血管内介入治疗取出下腔静脉滤器。在取出下腔静脉滤器之前病人侧腰疼痛只有在支持治疗下才能缓解。考虑到取出支柱干预的风险,决定将栓塞支柱不予取出。下腔静脉滤器断裂是这些装置潜在的并发症。
患者为一名28岁的妇女,因右侧腰部疼痛而到急诊就诊。该患者既往有肾结石病史,以及10年前发生过深静脉血栓和肺栓塞,她放置了下腔静脉滤器。
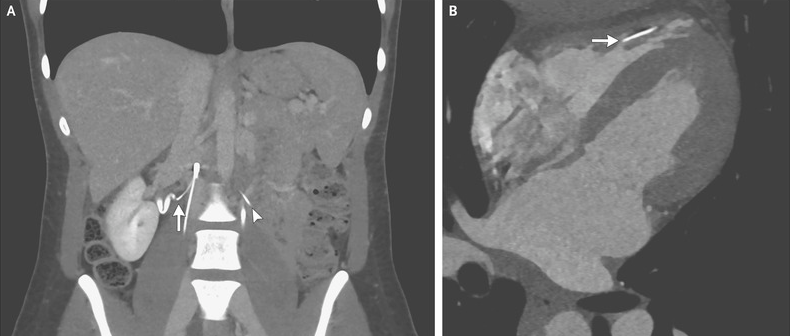
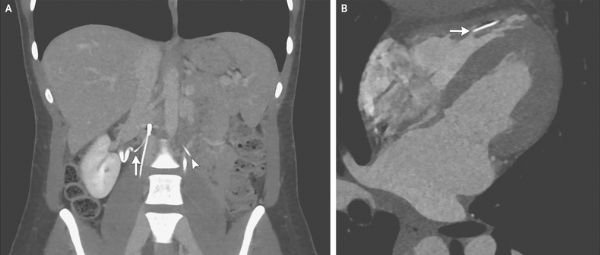
腹部计算机断层扫描显示一个支离破碎的带有多个穿孔支柱的下腔静脉滤器。一个支柱从右输尿管伸出约1毫米(如图A箭标所示)。这一发现是否与腰痛有关尚不清楚。另外两个支柱发生断裂、栓塞,其中一个位于左椎前间隙(如图A箭头所示),另一个位于右心室。心脏CT血管造影显示支架内无穿孔的右心室小梁(如图B箭头所示)。
该患者经血管内介入治疗取出下腔静脉滤器。在取出下腔静脉滤器之前病人侧腰疼痛只有在支持治疗下才能缓解。考虑到取出支柱干预的风险,决定将栓塞支柱不予取出。下腔静脉滤器断裂是这些装置潜在的并发症。
在过滤器取出后进行随访以及术后随访1年,病人感觉良好,并且正在接受临床监护。
原始出处:
Laura D. Flannery,et al. Embolization of Struts from an Inferior Vena Cava Filter. N Engl J Med 2018; http://www.nejm.org/doi/full/10.1056/NEJMicm1710700
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#下腔静脉#
0
#静脉#
21
#腔静脉滤器#
40
学习谢谢分享
45
谢谢分享.学习了
61
好文章.学习学习
61
学习学习.了解了解
40