NEJM:3期临床试验证实中国手足口病疫苗安全有效
2014-03-06 xiaorong699 dxy
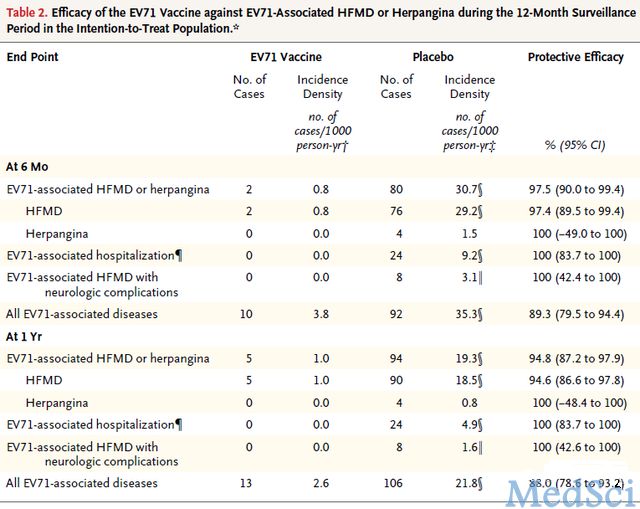
肠道病毒71型(EV71)是引发手足口病或咽峡炎的主要病原体之一。2008年EV71病毒在中国流行,共造成49万人感染,126人死亡。这些感染和死亡病例集中在3岁以下的婴幼儿。目前世界上尚无针对EV71病毒的特异性疫苗。 来自江苏省疾病预防控制中心、中国疾病预防控制中心、中国食品药品检定研究院等多家机构的科研人员研制出一种基于Vero细胞、以氢氧化铝为佐剂的EV71灭活疫苗。1期和2期临
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








好好学习一下
66
好好学习一下
50
好好学习一下
67
#3期临床#
40
#手足口#
36
#3期临床试验#
25