Stroke:脑淀粉样血管病临床和神经影像学标志物的患病率
2022-03-12 MedSci原创 MedSci原创
大约一半的CAA患者队列观察到有脑微出血、皮质浅表铁质沉着症、轻度认知障碍、痴呆、ICH或短暂的局灶性神经系统发作。皮质浅表铁质沉着症是唯一与ICH复发率较高相关的神经影像学标志物。
脑淀粉样血管病(CAA)患者的临床和神经影像学表现的患病率数据有限。近日,心血管疾病领域权威杂志Stroke上发表了一篇研究文章,研究人员试图确定CAA患者临床表型和放射学标志物的患病率。

研究人员对包括CAA患者在内的研究进行了系统回顾和荟萃分析,主要纳入了评估临床表型和神经影像学标志物患病率可用的研究。研究人员根据(1)回顾性或前瞻性研究设计和(2)可能或未指定的CAA状态进行了敏感性分析。研究人员使用随机效应模型汇总患病率,并使用Cochran Q和I2统计量评估异质性。

研究人员确定了12项前瞻性研究和34项回顾性研究,纳入了7159名CAA患者。汇总的患病率是脑微出血(52%[95%CI为43%-60%];I2=93%),皮质浅表铁质沉着症(49%[95%CI为38%-59%];I2=95%)、痴呆或轻度认知障碍(50%[95%CI为35%-65%];I2=97%)、脑出血(ICH;44%[95%CI为27%-61%];I2=98%),短暂的局灶性神经系统发作(48%;10项研究[95%CI为29%-67%];I2=97%),腔隙性梗塞(30%[95%CI为25%-36%];I2=78%),位于半卵圆中心(56%[95%CI为44%-67%];I2=88%)和基底节(21%[95%CI为2%-51%]);I2=98%)的高等级血管周围间隙,以及白质高信号伴中度或重度Fazekas评分(53%[95%CI为40%-65%];I2=91%)。
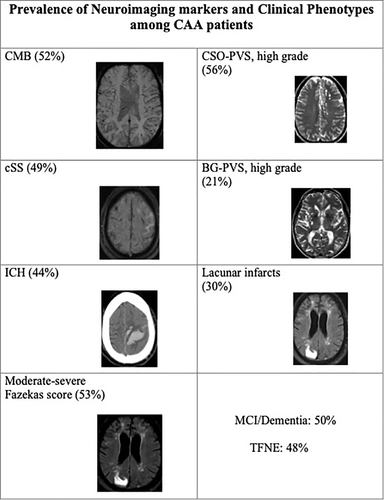
唯一与ICH复发率较高相关的神经影像学标志物是皮质浅表铁质沉着症(比值比为1.57[95%CI为1.01-2.46];I2=47%)。敏感性分析表明,与前瞻性研究相比,回顾性研究中ICH(53% vs. 16%;P=0.03)和短暂性局灶性神经系统发作(57% vs. 17%;P=0.03)的患病率更高。基于CAA状态的患病率之间没有差异。
由此可见,大约一半的CAA患者队列观察到有脑微出血、皮质浅表铁质沉着症、轻度认知障碍、痴呆、ICH或短暂的局灶性神经系统发作。皮质浅表铁质沉着症是唯一与ICH复发率较高相关的神经影像学标志物。未来在明确定义的CAA队列中进行的基于人群的研究有必要证实这一研究的结果。
原始出处:
Konark Malhotra.et al.Prevalence of Clinical and Neuroimaging Markers in Cerebral Amyloid Angiopathy: A Systematic Review and Meta-Analysis.stroke.2022.https://www.ahajournals.org/doi/10.1161/STROKEAHA.121.035836
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#神经影像#
38
#标志物#
39
#血管病#
0
#脑淀粉样#
57
#患病率#
30
#脑淀粉样血管病#
42