为何有些病毒那么热衷于通过精液传播?
2016-02-25 sunshine&KL MedSci原创
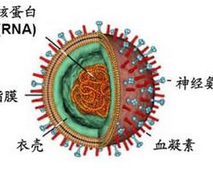
为何有些病毒特别容易经精液传播本周,美国疾病控制和预防中心再次警告,Zika病毒可通过性传播。除此之外,男性患者病毒清除后仍可在其精液中存留数周。在此之前研究人员就已警告过病毒可在精液中存活很长的时间。埃博拉疫情爆发期间,研究人员发现,患者康复后病毒仍可在其精液中持续存在数月。有些病毒,如HIV,可通过精液有效传播,但是却不会通过其他的体液传播,如眼泪或尿液。这就提出了一个问题:精液有何特别之处?
本周,美国疾病控制和预防中心再次警告,Zika病毒可通过性传播。除此之外,男性患者病毒清除后仍可在其精液中存留数周。
原始出处:
Julia Belluz.The surprising reason some diseases spread so effectively through semen.Science & Health.24 February 2016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












好好学习
119
学习了,原来是于血睾丸屏障有关啊
141
布置作业了
132
看看吧
131
#精液#
40
营养丰富
120
危险
75
额,已阅
70