J Thorac Oncol:肺癌患者再发第二原发肺癌的风险有多大
2017-10-30 肿瘤资讯编辑部 肿瘤资讯
肺癌是全球发病率和死亡率最高的肿瘤,近年来,随着诊断技术和治疗手段的进展,肺癌整体的生存期得到显着的延长。随着患者生存期的研究,临床上出现第二原发肺癌的机率也相应增加。那么,对于原发性肺癌患者,再发第二原发肺癌的风险有多大呢?不同临床特征的患者,发病风险是否有差异?近期发布在《Journal of Thoracic Oncology》的一项研究通过回顾性分析SEER数据库,对这一问题进行了回答。
背景
肺癌是美国癌症病死率最高的瘤种,对于首次诊断为原发性肺癌(initial primary lung cancer, IPLC)患者,后续仍持续面临第二原发肺癌(second primary lung cancer, SPLC)的风险。SPLC定义为,接受了以根治为目的治疗后的IPLC患者,再发新的原发性肺癌。SPLC的发病风险为每人每年1-2%。IPLC患者再发SPLC后,预后较差。既往,在国家肺癌筛查试验(NLST)中,并没有将既往罹患肺癌的患者纳入筛查人群。目前的癌症随访指南中也没有提及对SPLC的筛查。既往关于SPLC的研究数据都是来自对部分IPLC患者的分析,如特定分期或接受特定治疗的患者,因此,总的SPLC发生率仍然未知。鉴于目前早期肺癌患者的预后越来越好,有必要对SPLC的发生率进行一个全面清晰的了解。
在SEER数据库中,定义为多原发肺癌的依据为:1. 不同组织学类型;2. 每侧肺叶一个孤立的肿瘤;3. 两个肿瘤的间隔时间超过3年;4. 在诊断为原位癌60天后再发浸润性癌。本研究旨在通过分析SEER数据库,来评估SPLC的发生率。并分析患者不同临床特征(如性别,年龄,种族,组织学类型等)发生SPLC的累积风险。
方法
研究收集了SEER-13登记处有完整长期随访数据资料的患者。入组1992-2007年期间第一次诊断为原发性肺癌,年龄20岁或以上的患者,对SPLC的随访至2012年。记录患者诊断时的年龄,诊断日期,性别,种族,组织学类型,诊断为IPLCs和SPLCs的分期,两次诊断的间隔。患者的年龄分为4个区间:20-49岁,50-59岁,60-69岁和70岁或以上。IPLC的诊断时间分为3个时段:1992-1996年,1997-2001年,2002-2007年。种族分为黑人,白人和其他。组织学类型分为4类:鳞癌,腺癌,其他NSCLC,SCLC。肿瘤的分期分为:局部,区域,远处,未知。
通过比较SPLC的发生率和一般人群的发生率来计算标准化发病比(standardized incidence ratio,SIR)和95%CI。研究分别计算了总体人群的SIRs以及不同性别,种族,年龄组,组织学类型,SEER数据库记录的分期,IPLC诊断年份等不同组别患者的SIR。
结果
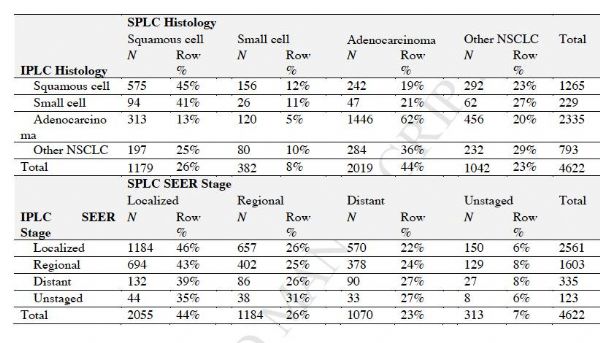
1. 临床特征分析
SEER 13数据库中,1992年至2007年,共156494例首次诊断为原发性肺癌的患者。其中男性患者占54%(83971例),女性患者占46%(72523)。80%的患者都为高加索人,NSCLC和SCLC的比例分别为88%的12%。SEER数据库中的分期为:远处38%,局部32%,区域23%,未知7%。3%(4622例)的患者继发SPLC。所有入组人群和继发SPLC的患者临床特征对比如下。
表1. 所有入组人群和继发SPLC的患者临床特征对比
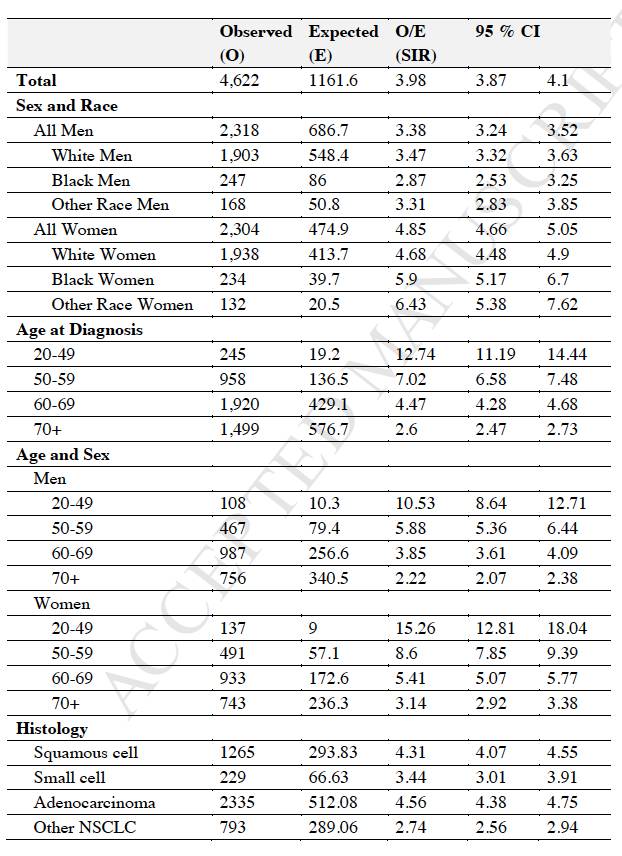
2. SIR分析
在所有年龄组和不同种族患者中,女性的SIR最高,其中最年轻组(年龄20-49岁)的女性队列,SIR最高(SIR=15.26; 95% CI 12.81 – 18.04)。无论是男性还是女性,随着IPLC诊断年份的增加,SIR增高。不同临床特征患者继发SPLC的SIR总结见下表。
表2: 不同临床特征患者继发SPLC的SIR
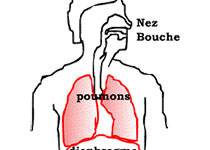
3. 组织学和分期
在IPLC的主要组织学类型为腺癌和鳞癌(共占59%),SPLC中腺癌和鳞癌患者比例更高,占78%。IPLC为腺癌的患者,继发的SPLC多为腺癌(62%);IPLC为鳞癌和SCLC的患者,继发的SPLC多为鳞癌(分别为45%和41%)。仅8%的SPLC为鳞癌,这一比例较IPLC患者更高(5%)。
大多数继发SPLC的患者为局部IPLC(55%),有一小部分患者患者为远处IPLC(见表1)。大多数(56%)的SPLCs诊断时为晚期疾病(区域或远处)或分期未知,仅44%的SPLCs为局部疾病。IPLC不同组织学和分期患者继发SPLC的特征总结见下表。
表3. IPLC不同组织学和分期患者继发SPLC的特征总结
随着时间延长,SPLC的累积风险增加,其中男性的风险稍高于女性。男性和女性IPLC患者,继发SPLC的中位时间分别为 59岁和62岁。总体人群中,继发SPLC的风险为每人每年1.10%,且随着时间的延长,并没有观察到发病风险出现平台期。
图1. 随时间变化男性和女性继发SPLC的风险
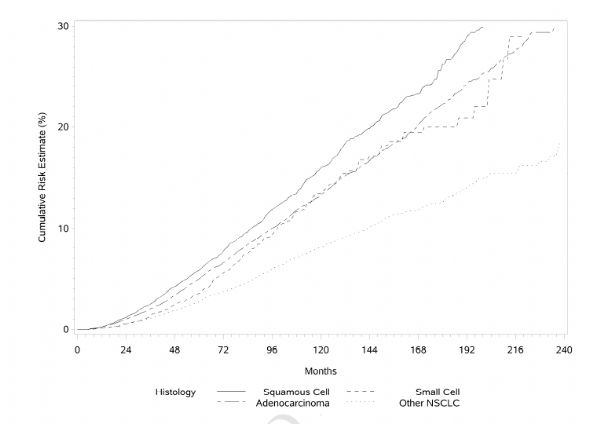
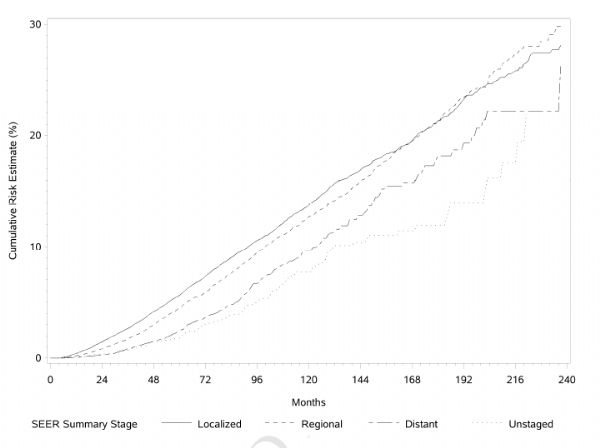
此外,IPLC为鳞癌和初始诊断为局部疾病的患者,继发SPLC的累积风险更高。
图2. IPLC不同病理类型患者继发SPLC的累积风险
图3. IPLC不同分期患者继发SPLC的累积风险
结论和点评
本研究通过对SEER数据库的分析发现诊断为原发性肺癌的患者有继发SPLC的风险,且发病风险随时间延长而增加。出现SPLC的中位时间为5年。此外,大部分的SPLC诊断时不是早期。这一研究结果提示,对于原发性肺癌患者在随访过程中,除了要监测疾病是否复发,还要关注患者有继发SPLC的风险,如应该进行一些影像学的复查等。
Thakur MK, Ruterbusch , Schwartz AG, et al.Risk of Second Lung Cancer in Patients with Previously Treated Lung Cancer: Analysis of Surveillance, Epidemiology and End Results (SEER) Data. Journal of Thoracic Oncology (2017), doi: 10.1016/j.jtho.2017.09.1964.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncol#
19
#THORAC#
30
#第二原发肺癌#
27
#肺癌患者#
21
学习了
38
学习一下谢谢分享
38