Asia Pac Allergy:永久性过敏性鼻炎患者中,血清25-羟甲基维生素D与血嗜酸细胞负相关
2017-11-09 AlexYang MedSci原创
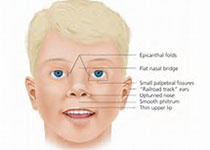
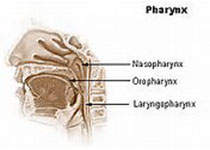
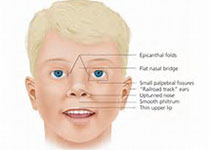
维生素D和过敏性鼻炎(AR)之间的关系仍旧不清楚。最近,有研究人员通过在患有AR的病人中检测血清25-羟甲基维生素D(25(OH)D)调水平、血嗜酸细胞和维生素D受体(VDR)在鼻粘膜上的表达调查了它们之间的关系。研究包括了32名患有永久性过敏性鼻炎的病人和25名对照。研究人员通过酶联免疫试验检测了血清25(OH)D的水平,利用自动化的血液系统检测了外周血嗜酸细胞,然而在下鼻甲粘膜中VDR的表达则
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ASIA#
29
#过敏性#
34
#ALL#
35
#负相关#
31
学习了.非常好的文章
71
学习了.涨知识
62