Eur Respir J:右心房功能与右心室舒张僵硬度相关:肺动脉高压中右心房-右心室的相互作用
2021-11-12 刘少飞 MedSci原创
肺动脉高压 (PAH) 患者的右心房 (RA) 功能和右心室 (RV) 舒张期硬度发生了改变。本研究评估了 RV 舒张期硬度对 RA-RV 相互作用的影响。

右心室(RV)适应对于肺动脉高压(PAH)患者至关重要,因为RV衰竭是症状和死亡率的主要决定因素。心室适应的标志之一是肥大,以心室硬化为表现,胶原沉积和肌联蛋白磷酸化的变化加剧了心室硬化。一些硬化可能是有益的,因为它可以防止右心室的明显扩张,但过度硬化可能会产生不利影响。 RV 舒张期僵硬程度与疾病严重程度的其他参数相关,并且是死亡率的预测因子。它也可能影响右心房 (RA) 功能,正如最近 RV 舒张硬度与腔静脉回流和 RA 纵向应变的相关性所表明的那样。然而,尚不清楚 RA 功能的变化是反映 RA 收缩受损,还是作为 RV 舒张僵硬的(可能可逆的)结果发展。我们使用了一种综合方法,将治疗前后 PAH 患者的 RA 和 RV 应变测量与压力-容积分析相结合,以评估 RA-RV 相互作用和不同级别 RV 舒张硬度下的腔静脉回流,以回答以下临床问题:
1.RA 功能的变化是 RV 舒张期僵硬的结果还是反映了 RA 收缩受损?
2.严重的 RV 舒张期僵硬在多大程度上是可逆的,逆转是否会导致 RA-RV 相互作用的改善和腔静脉回流的减少?
研究方法:
评估了 2002 年 12 月至 2019 年 5 月在荷兰阿姆斯特丹大学医学中心(PAH 三级转诊中心)诊断出的特发性、遗传性或结缔组织病 (CTD) 相关 PAH 患者(n=178)。患者在基线和随访时在右心导管插入术的两周内接受了心脏磁共振成像(CMR)。 基线用药、RV 压力曲线质量差或 CMR 图像是排除标准 (n=84)。 这导致 n = 94 名患者根据中位舒张末期弹性 (Eed) 分为两个亚组,高 Eed 识别具有严重 RV 舒张期僵硬度的 PAH 患者。 将低或高舒张末期弹性 (E ed ) PAH 患者 (n=94) 与对照组 (n=31) 进行比较。在 n = 62 名患者中评估了治疗反应。确定了 RV 和 RA 纵向应变、RA 排空和 RV 充盈,并将舒张期分为被动和主动阶段。
研究结果:
基线特征
研究人群包括 63 名特发性、9 名遗传性和 25 名 CTD-PAH 患者。 患者的年龄为 58±18 岁,主要是女性 (65%)。 平均而言,患者的 Eed (0.70±0.41 mmHg/ml) 是对照组 (0.20±0.08 mmHg/ml) 的 3.5 倍,表明显着的 RV 舒张僵硬度。 根据 0.63 mmHg/ml 的中值,将患者分为低 Eed 组和高 Eed 组。
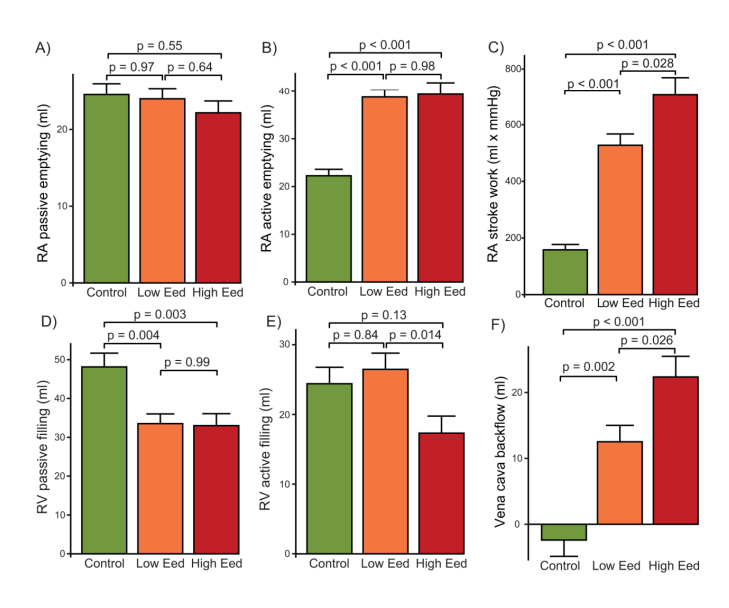
随着Eed 的增加,RA 和RV 被动应变减少,而主动应变得以保留。
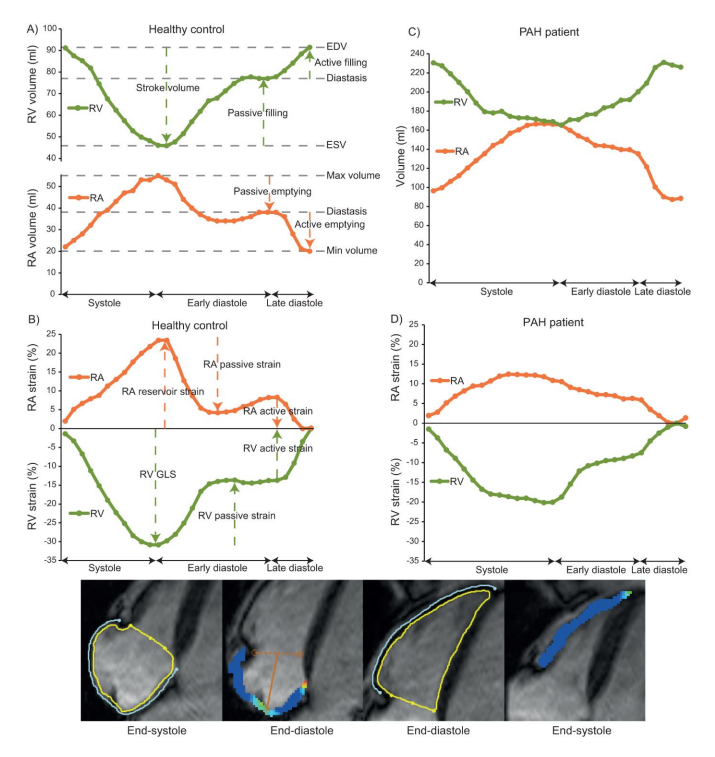
与对照组相比,患者的 RV 被动充盈较低,但 RA 主动排空和 RA 输出量较高。

高 E ed患者的RV 主动充盈较低,导致腔静脉回流较高。
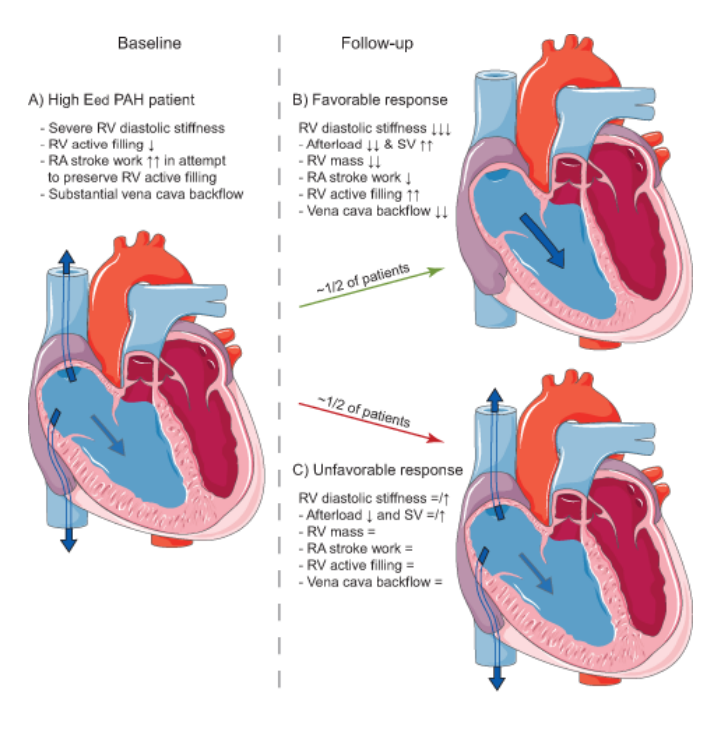
治疗后,半数高 E ed患者的E ed降低,与 E ed保持高的患者相比,后负荷、RV 质量和腔静脉回流的减少幅度更大,RV 主动充盈和每搏输出量的改善更大。
研究结论及启示:
在PAH中,RA功能与RV功能的变化有关。尽管RA输出量做功增加,严重的 RV 舒张期僵硬与 RV 主动充盈减少和腔静脉回流增加有关。在 50% 的高基线 E ed患者中,尽管进行了治疗,但舒张僵硬度仍然很高。E ed减少与后负荷大幅减少、右室主动充盈增加和腔静脉回流减少同时发生。
文献出处:
Wessels JN, Mouratoglou SA, van Wezenbeek J, Handoko ML, Marcus JT, Meijboom LJ, Westerhof BE, Jan Bogaard H, Strijkers GJ, Vonk Noordegraaf A, de Man FS. Right atrial function is associated with RV diastolic stiffness: RA-RV interaction in pulmonary arterial hypertension. Eur Respir J. 2021 Nov 11:2101454. doi: 10.1183/13993003.01454-2021. Epub ahead of print. PMID: 34764180.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#相互作用#
49
#右心房#
54
#动脉高压#
30
学习到了新知识。
63
#互作#
39
#右心室#
45
#心房#
43