J Clin Oncol:雷莫芦单抗联合派姆单抗治疗晚期非小细胞肺癌
2022-06-05 MedSci原创 MedSci原创
雷莫芦单抗联合派姆单抗治疗可显著提高既往治疗过的晚期NSCLC患者的总生存率
有PD-L1表达的转移性非小细胞肺癌(NSCLC)的一线治疗通常单用程序性死亡受体1(PD-1)或其配体(PD-L1)抑制剂,或联合化疗或细胞毒性T淋巴细胞-相关抗原4抑制。但是,晚期NSCLC患者对免疫检查点抑制剂(ICI)的耐药性仍然是临床面临的一重要挑战。ICI与血管内皮生长因子(VEGF)/VEGF受体抑制相结合在多种肿瘤中产生了有希望的结果。
本研究是一项随机的、肺-MAP、非匹配的2期亚组研究,招募了既往采用ICI治疗和铂类化疗过的、在ICI开始治疗84天内发生进展的、生物标志物匹配的NSCLC患者,随机分成两组,予以雷莫芦单抗+派姆单抗(RP)或调查者选择的标准疗法(SOC:多西他赛/雷莫芦单抗、多西他赛、吉西他滨和培美曲塞)。主要终点是总生存率。次要终点包括客观缓解率、缓解持续时间、无进展生存期和毒性。
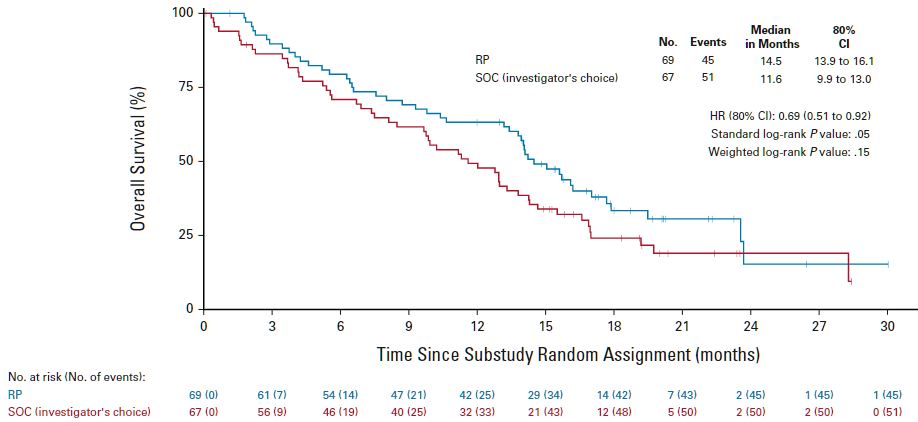
两组的总生存率
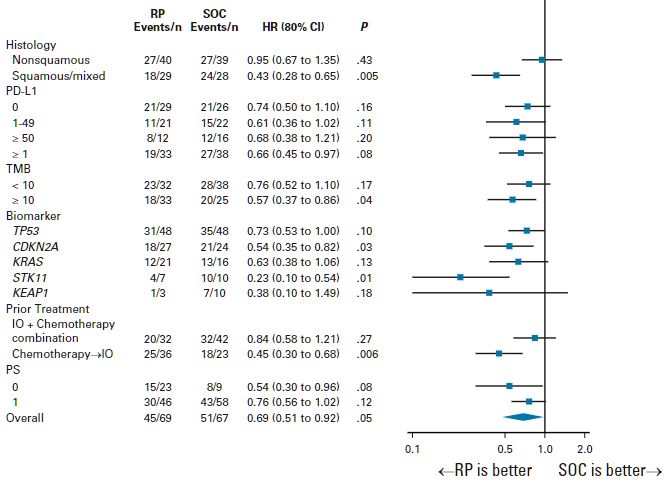
在招募的166位患者中,有136位被纳入分析(RP组 69位,SOC组 67位)。与SOC组相比,RP组患者的总生存率显著提高(HR 0.69, p=0.05)。PR组和SOC组的中位无进展生存期分别是14.5个月和11.6个月。在大部分亚组中均观察到RP组相比于SOC组的OS优势。
总生存率的亚组分析
两组间的无进展生存期(HR 0.86, p=0.25)和缓解率(RP vs SOC:22% vs 28%,p=0.19)均相近。RP组和SOC组分别有42%和60%的患者发生了3级及以上的治疗相关不良反应。
综上,该研究结果显示,与标准疗法相比,雷莫芦单抗联合派姆单抗治疗可显著提高既往接受化疗和ICI治疗过的晚期NSCLC患者的总生存率,而且无新的安全性问题。
原始出处:
Karen L. Reckamp, et al. Phase II Randomized Study of Ramucirumab and Pembrolizumab Versus Standard of Care in Advanced Non–Small-Cell Lung Cancer Previously Treated With Immunotherapy—Lung-MAP S1800A. Journal of Clinical Oncology. June 03, 2022. https://ascopubs.org/doi/full/10.1200/JCO.22.00912
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Oncol#
26
#非小细胞#
29
#派姆单抗#
64
学习
31