Sci Transl Med.:MG53蛋白可治疗实验性肌肉萎缩
2012-07-03 bo 生物谷
6月20日,Sci Transl Med杂志报道了一种新的针对细胞膜损伤修复的治疗性蛋白MG53。 mitsugumin53(MG53),是一种肌肉特异性tripartite motif family (TRIM)家族蛋白(该家族蛋白常含三个特定模序结构,分别被称为RING指,B-BOX,和卷曲结构域。它们共同作用结合在细胞不再需要的蛋白质上,将这些蛋白带上泛素标记以便降解),也是一种细胞膜修复
6月20日,Sci Transl Med杂志报道了一种新的针对细胞膜损伤修复的治疗性蛋白MG53。
mitsugumin53(MG53),是一种肌肉特异性tripartite motif family (TRIM)家族蛋白(该家族蛋白常含三个特定模序结构,分别被称为RING指,B-BOX,和卷曲结构域。它们共同作用结合在细胞不再需要的蛋白质上,将这些蛋白带上泛素标记以便降解),也是一种细胞膜修复机制的重要组成部分。该研究旨在探讨,针对MG53功能的干预,在组织修复和再生医学中的转化医学价值。
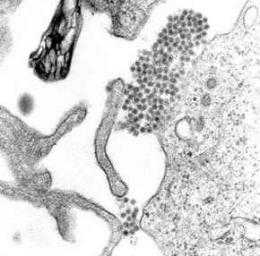
虽然天然MG53蛋白主要局限于骨骼肌和心肌组织,但在非肌肉细胞中过表达MG53也可发挥防止细胞损伤的作用。除了MG53在细胞内的作用,MG53也可感知损伤细胞膜所发出的信号。这使得在细胞外部给予重组MG53蛋白可修复细胞膜损伤。从大肠杆菌发酵纯化得到的重组人MG53(rhMG53)蛋白质,对化工,机械,或紫外线造成的肌肉和非肌肉细胞损伤,可提供剂量依赖性的保护作用。
在mdx肌营养不良小鼠模型中,通过多种途径注射rhMG53可降低肌肉病变。研究数据支持靶向细胞膜修复的再生医学观念,并提示MG53蛋白是一种大有前景的细胞膜修复缺陷人类疾病的治疗生物试剂。

doi:10.1016/j.cell.2011.10.017
PMC:
PMID:
Recombinant MG53 Protein Modulates Therapeutic Cell Membrane Repair in Treatment of Muscular Dystrophy
Noah Weisleder1,2,*, Norio Takizawa2, Peihui Lin1, Xianhua Wang3, Chunmei Cao3, Yan Zhang3, Tao Tan2, Christopher Ferrante2, Hua Zhu1, Pin-Jung Chen2, Rosalie Yan2, Matthew Sterling1, Xiaoli Zhao1, Moonsun Hwang1, Miyuki Takeshima4, Chuanxi Cai1, Heping Cheng3, Hiroshi Takeshima4, Rui-Ping Xiao3 and Jianjie Ma
Mitsugumin 53 (MG53), a muscle-specific TRIM family protein, is an essential component of the cell membrane repair machinery. Here, we examined the translational value of targeting MG53 function in tissue repair and regenerative medicine. Although native MG53 protein is principally restricted to skeletal and cardiac muscle tissues, beneficial effects that protect against cellular injuries are present in nonmuscle cells with overexpression of MG53. In addition to the intracellular action of MG53, injury to the cell membrane exposes a signal that can be detected by MG53, allowing recombinant MG53 protein to repair membrane damage when provided in the extracellular space. Recombinant human MG53 (rhMG53) protein purified from Escherichia coli fermentation provided dose-dependent protection against chemical, mechanical, or ultraviolet-induced damage to both muscle and nonmuscle cells. Injection of rhMG53 through multiple routes decreased muscle pathology in the mdx dystrophic mouse model. Our data support the concept of targeted cell membrane repair in regenerative medicine, and present MG53 protein as an attractive biological reagent for restoration of membrane repair defects in human diseases.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#实验性#
34
#Transl#
38
#TRA#
29
#萎缩#
35
#肌肉萎缩#
38
#Med#
25